A groundbreaking study published in Science China Life Sciences unveils a pivotal mechanism driving the resilience and aggressiveness of glioblastoma (GBM), the most lethal form of brain cancer, under hypoxic conditions. For decades, researchers have grappled with the challenge posed by GBM’s median survival rate, stubbornly fixed at approximately 15 months. This persistence is largely attributed to hypoxic niches within tumors that nurture drug-tolerant, invasive cancer cell populations. While the hypoxia-inducible factor (HIF) pathway has long been considered the central player in cellular adaptation to oxygen deprivation, new research led by Professor Xudong Wu at Tianjin Medical University reveals an alternative HIF-independent molecular axis critical for GBM proliferation and survival.
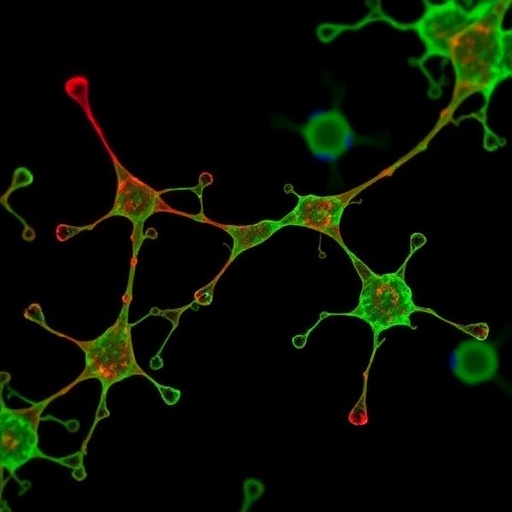
Professor Wu’s team employed an arsenal of innovative techniques including single-cell imaging, molecular biochemistry, and patient-derived tumor models, enabling them to dissect the response of GBM cells to acute oxygen deprivation with unprecedented granularity. Their findings uncover a previously unrecognized role for the epigenetic enzyme PRMT2, which, contrary to prior assumptions, is rapidly mobilized within minutes of hypoxia onset. PRMT2 migrates into specialized, membrane-less nuclear assemblies known as “transcriptional condensates.” These liquid-like droplets serve as reaction chambers concentrating transcriptional machinery, facilitating swift and robust gene activation essential for tumor adaptation and survival under stress conditions.
The biochemical underpinnings of PRMT2’s activation involve a post-translational modification catalyzed by cyclin-dependent kinase 9 (CDK9). Specifically, phosphorylation at serine-12 on PRMT2 both drives its retention within these transcriptional condensates and significantly enhances its methyltransferase activity. This hyperactivation enables PRMT2 to deposit dimethylation marks—specifically the H3R8me2a mark—on histone tails, implementing an epigenetic program that stimulates genes responsible for angiogenesis and metabolic reprogramming critical for hypoxia endurance and tumor aggressiveness.
Adding a compelling genetic dimension to their mechanistic insight, the team identified a naturally occurring PRMT2 mutation (G5S) in a subset of GBM patients. This mutation structurally mimics the phosphorylation event induced by CDK9, rendering PRMT2 constitutively hyperactive and avidly condensed within nuclear droplets. The presence of this mutation correlates with enhanced aggressiveness and poorer clinical prognosis, positioning it as a promising genetic biomarker for stratifying patient risk and tailoring therapeutic interventions.
Perhaps most strikingly from a translational perspective, the study reveals that targeting the CDK9-PRMT2 axis is therapeutically feasible with TG02, an orphan drug previously trialed in glioma contexts. TG02 exerts its pharmacological effects by inhibiting CDK9, thereby preventing the phosphorylation-dependent condensation and activation of PRMT2. Remarkably, nanomolar concentrations of TG02 were sufficient to abolish the H3R8me2a histone mark and suppress the hypoxia-induced gene expression program, highlighting the drug’s potent epigenetic modulatory capacity.
The therapeutic implications were rigorously tested in vivo using murine models harboring temozolomide (TMZ)-resistant GBM tumors. When administered as a monotherapy, TG02 exhibited modest tumor-suppressive effects. However, combined with TMZ, the current standard-of-care chemotherapy, TG02 synergistically induced pronounced tumor regression, effectively dismantling the hypoxia-mediated chemotherapy resistance. This combinatorial strategy significantly doubled the survival of treated animals without incurring additional systemic toxicity, implying a favorable therapeutic index.
Molecular analyses of tumors treated with the TG02 plus TMZ regimen illustrated a dramatic disruption of the hypoxic microenvironment’s protective shield. This collapse of hypoxia-driven resistance pathways reinstated TMZ sensitivity, even within the notoriously refractory tumor core. These findings underscore the potential of epigenetic interference in overcoming one of the most formidable barriers in GBM treatment—intratumoral hypoxia-induced chemoresistance.
Professor Wu emphasizes that this research exemplifies a broader biological principle: transcriptional condensates act as catalysts that amplify epigenetic enzyme function, creating potentiated signaling hubs that can be effectively targeted pharmacologically. By exploiting the vulnerabilities of phase-separated nuclear compartments, TG02 offers an immediately actionable avenue for clinical intervention, providing renewed hope for patients afflicted by this devastating malignancy.
This study also raises critical questions for future research. The dynamic interplay between transcriptional condensates and epigenetic modifiers such as PRMT2 during tumor progression remains largely unexplored, offering fertile ground for the discovery of additional therapeutic targets. Moreover, the identification of a mutation-driven hyperactivation mechanism invites investigation into personalized medicine approaches that could leverage genetic profiling to inform treatment selection.
Moving forward, the research team is advancing preclinical studies to refine dosing strategies and evaluate long-term outcomes associated with the TG02 and TMZ combination. These efforts aim to accelerate the translation of their findings into clinical trials, potentially transforming the therapeutic landscape for GBM patients.
In conclusion, this work dramatically expands the understanding of hypoxia adaptation mechanisms in glioblastoma, revealing an uncharted HIF-independent epigenetic program orchestrated by PRMT2 within transcriptional condensates. The therapeutic exploitation of this axis through the repurposing of TG02, particularly in synergy with temozolomide, represents a paradigm shift in overcoming chemoresistance and improving survival outcomes for one of the most intractable cancers.
Subject of Research: Glioblastoma hypoxia adaptation, epigenetic regulation, PRMT2, transcriptional condensates, chemoresistance mechanisms.
Article Title: HIF-Independent Epigenetic Circuitry through PRMT2 Drives Hypoxia Adaptation and Chemoresistance in Glioblastoma.
Web References: https://doi.org/10.1007/s11427-025-2959-x
References: (Details not provided in the original content)
Image Credits: (Details not provided in the original content)
Keywords: Glioblastoma, hypoxia, PRMT2, transcriptional condensates, CDK9, epigenetics, H3R8me2a, TG02, chemoresistance, temozolomide, tumor microenvironment, orphan drug.
Tags: epigenetic role of PRMT2glioblastoma cancer resistanceHIF-independent molecular pathwayshypoxic conditions in tumorsinnovative techniques in cancer researchmechanisms of drug tolerance in GBMoxygen deprivation effects on tumorssingle-cell imaging in tumor studiesstrategies to combat glioblastoma aggressivenesstranscriptional condensates in cancertumor microenvironment and survivaltumor stress droplets