In a groundbreaking study recently published in Nature Communications, researchers have unveiled intricate details of SARS-CoV-2 infection dynamics within an exceptional clinical context: a lung transplant recipient exhibiting a major histocompatibility complex class I (MHCI) mismatch. This discovery not only advances our understanding of viral-host interactions in immunologically complex environments but could also pave the way for refined therapeutic strategies in transplant medicine amid ongoing viral pandemics.
The investigation centered on a lung transplant patient whose donor tissue was MHCI mismatched, a scenario that poses unique immunological challenges. MHCI molecules play a crucial role in presenting viral peptides to cytotoxic T lymphocytes (CTLs), triggering targeted immune responses. When donor and recipient MHCI profiles do not align, immune surveillance mechanisms face an altered landscape, potentially influencing viral replication and clearance rates. This setting provided a rare opportunity to dissect how SARS-CoV-2 behaves under such altered immunological constraints.
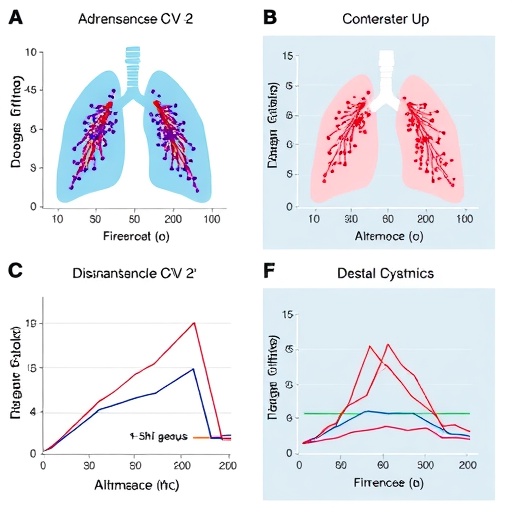
Utilizing longitudinal sampling and advanced virological assays, the research team monitored viral RNA abundance across several post-infection intervals, capturing the ebb and flow of SARS-CoV-2 replication within the recipient’s transplanted lung tissue. The data revealed a distinct infection kinetic profile, marked by prolonged viral persistence despite clinical recovery markers. This contrasted with typical infection courses observed in immunocompetent hosts, where viral load tends to decline more rapidly.
The study employed high-resolution sequencing techniques to map the viral genomic landscape throughout the infection timeline. Intriguingly, mutational patterns emerged that suggested selective pressures unique to the environment shaped by MHCI mismatch. Variants harboring mutations in the spike protein receptor-binding domain (RBD) appeared during prolonged infection phases, hinting at viral adaptation attempts to escape immune detection or harness altered cellular entry mechanisms.
Immunological analyses unveiled disrupted CTL responses attributable to the MHCI mismatch. Recipient-derived cytotoxic T cells, which rely on MHCI presentation to recognize infected cells, exhibited diminished efficacy in identifying donor lung tissue harboring SARS-CoV-2. This compromised immune surveillance likely contributed to the observed delay in viral clearance. Moreover, compensatory immune pathways, such as natural killer (NK) cell activity, were evaluated, revealing partial, albeit insufficient, engagement against infected cells.
The patient’s immunosuppressive regimen, essential to prevent organ rejection, added another layer of complexity. Researchers meticulously documented how various immunosuppressants modulated immune cell populations and influenced viral load dynamics. The findings underscored a delicate balance between preventing graft rejection and maintaining antiviral defenses, a clinical conundrum intensified during pandemics involving novel respiratory pathogens.
Importantly, the authors highlighted the implications of prolonged viral replication in transplanted tissue for viral evolution and potential emergence of escape variants. The sustained infection window created a reservoir wherein SARS-CoV-2 could undergo accelerated mutagenesis, potentially fostering variants with enhanced transmissibility or immune evasion capabilities. This has profound consequences not only for individual patient outcomes but also for public health strategies addressing immunocompromised populations.
The synergy of virology, immunology, and transplant medicine in this research underscores the need for multidisciplinary approaches to tackle infectious diseases in specialized patient cohorts. The study advocates for tailored antiviral regimens and vigilant monitoring protocols to mitigate risks associated with prolonged viral presence in transplanted organs, especially when MHCI incompatibility is involved.
Methodologically, the team harnessed single-cell RNA sequencing to map cellular responses within the lung microenvironment, elucidating how infected epithelial cells and infiltrating immune populations interacted over time. These data illuminated the nuanced crosstalk between persistent virus and host cells, shedding light on pathways that could be targeted therapeutically to enhance viral clearance without jeopardizing graft viability.
Complementing molecular analyses, the researchers utilized advanced imaging modalities to visualize viral dissemination and immune cell infiltration in the lung graft. The dynamic interplay observed corroborated molecular findings and reinforced the concept that MHCI mismatching disrupts conventional immune containment of viral infections at the tissue level.
Given the ongoing challenges posed by SARS-CoV-2 variants worldwide, especially among vulnerable populations such as transplant recipients, these findings are timely and critical. They provide a framework for clinicians to anticipate infection trajectories, tailor immunosuppressive therapies, and potentially incorporate novel antiviral agents to prevent chronic infection and viral evolution inside immunocompromised hosts.
Moreover, this study contributes to a broader scientific dialogue about how host genetics and immune compatibility influence infectious disease outcomes. The unique setting of MHCI mismatch offers a natural experiment for unraveling the immunogenetic determinants of viral pathogenesis, with ramifications extending beyond COVID-19 and applicable to other viral infections threatening transplant patients.
Looking forward, the authors call for expanded investigations encompassing diverse transplant types and MHCI mismatch combinations, aiming to generalize these findings and refine patient management guidelines. Such efforts will be critical to fortifying health system resilience against emerging viral threats, ensuring that life-saving organ transplants do not become unintended sanctuaries for pathogen persistence.
In sum, this pioneering research delineates the complex landscape of SARS-CoV-2 infection within a MHCI-mismatched lung transplant recipient, advancing the frontier of knowledge at the intersection of virology, immunology, and transplant medicine. Its insights deepen our understanding of viral persistence mechanisms, highlight vulnerabilities in transplant immunology, and underscore the imperative for vigilant, personalized approaches in managing infections in immunologically intricate settings.
Subject of Research: SARS-CoV-2 infection dynamics in an MHCI-mismatched lung transplant recipient.
Article Title: SARS-CoV-2 infection dynamics in a MHCI-mismatched lung transplant recipient.
Article References:
Fuchs, J., Karl, V., Hettich, I. et al. SARS-CoV-2 infection dynamics in a MHCI-mismatched lung transplant recipient. Nat Commun 16, 8292 (2025). https://doi.org/10.1038/s41467-025-63681-y
Image Credits: AI Generated
Tags: COVID-19 research advancementscytotoxic T lymphocytes functionimmune response to SARS-CoV-2longitudinal sampling of viral RNAlung transplant immunologyMHCI mismatch implicationspersistent viral replication in transplantsSARS-CoV-2 infection dynamicstherapeutic strategies for lung transplant patientstransplant medicine and viral pandemicsviral-host interactions in transplantsvirological assays in transplant patients