In recent years, the intricate dialogue between cancer cells and their surrounding microenvironment has emerged as a critical determinant of tumor progression and therapeutic resistance. A groundbreaking study published in Cell Death Discovery unveils a novel molecular mechanism by which adipocytes, the fat-storage cells abundant in breast tissue, engage in a deleterious crosstalk with triple-negative breast cancer (TNBC) cells. This research, led by Ruan et al., sheds light on how adipocyte-derived interleukin 6 (IL6) and TNBC cell-secreted chemokine ligand 1 (CXCL1) conjointly activate the STAT3 and NF-κB signaling pathways, facilitating a potent communication axis that fuels tumor aggressiveness.
Triple-negative breast cancer represents one of the most formidable breast cancer subtypes, characterized by the absence of estrogen receptor, progesterone receptor, and HER2 amplification. This molecular profile renders it refractory to many targeted therapies, underscoring an urgent need to decipher the underlying biological complexities driving its malignant behavior. The tumor microenvironment, particularly the interplay between malignant cells and adipocytes in the mammary fat pad, has come under intense scrutiny as a vital contributor to such aggressiveness. Adipocytes, once considered passive bystanders, are now recognized as active participants that modulate cancer cell survival, invasion, and metabolic reprogramming via secreted factors and direct cellular crosstalk.
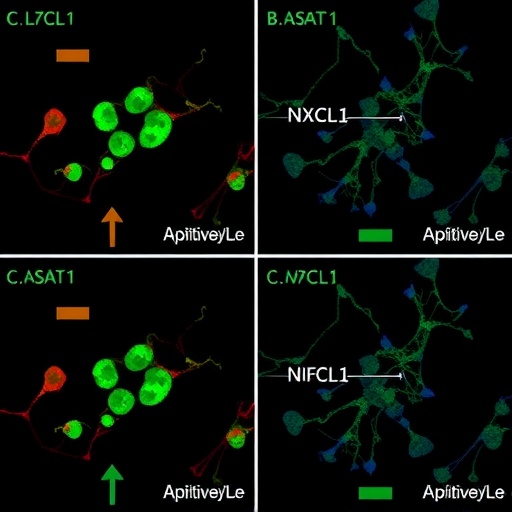
The current study meticulously examines the paracrine feedback loop mediated by IL6 and CXCL1 between adipocytes and TNBC cells. Using co-culture systems and patient-derived tumor samples, the authors demonstrate that IL6 emanating from adipocytes significantly elevates CXCL1 production in adjacent TNBC cells. This elevation of CXCL1, in turn, potentiates the activation of the STAT3 and NF-κB transcription factors, which are renowned for their roles in inflammatory signaling, cell proliferation, and survival. The co-activation of these pathways forms the molecular underpinning of enhanced tumor progression, metastasis, and potential chemo-resistance in TNBC.
.adsslot_fWHMS1ApQO{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_fWHMS1ApQO{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_fWHMS1ApQO{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
At a mechanistic level, the IL6/STAT3 axis has long been associated with inflammatory signaling within the tumor microenvironment, promoting a milieu conducive to neoplastic expansion. However, this study reveals the additional layer of CXCL1 as a pivotal chemokine that not only reinforces STAT3 signaling but also synergistically triggers NF-κB activity. NF-κB, a master regulator of immune and stress responses, orchestrates the transcription of genes involved in cell survival, angiogenesis, and metastatic dissemination. The mutual reinforcement of STAT3 and NF-κB pathways creates a self-sustaining loop, maximizing the oncogenic potential of triple-negative breast cancer cells.
From a therapeutic perspective, these findings open new avenues for disrupting the pathological dialog between adipocytes and TNBC cells. Targeting IL6 signaling pathways has been explored previously in cancer treatments, albeit with limited clinical success in breast tumors. The elucidation of CXCL1 as a key mediator offers an additional, promising target to mitigate the tumor-supportive microenvironment. The dual blockade of IL6 and CXCL1 signaling cascades, or their downstream effectors STAT3 and NF-κB, might yield synergistic results, hindering tumor progression and improving patient outcomes.
Moreover, these discoveries emphasize the importance of the microenvironmental context in cancer biology—how nonmalignant cells like adipocytes can be co-opted by malignant cells to facilitate invasive phenotypes. This refined understanding prompts a reconsideration of adipose tissue not merely as an energy reservoir but as an active participant in breast cancer pathogenesis. It further suggests that obesity and adiposity, which alter adipocyte function and inflammatory profiles, could directly influence TNBC progression through enhanced IL6 secretion and subsequent molecular cascades.
Additionally, the study employed advanced molecular biology techniques, including RNA sequencing and immunohistochemistry, to validate expression patterns of IL6 and CXCL1 in human TNBC specimens. These experimental approaches established a significant correlation between high cytokine levels and poor clinical prognosis, reinforcing the clinical relevance of their mechanistic findings. The robust data sets delineate a clear path forward for biomarker development and tailored interventions.
In a broader context, the IL6/CXCL1-driven co-activation of STAT3/NF-κB signaling pathways resonates with emerging paradigms of chronic inflammation as a cancer hallmark. This work exemplifies how the inflammatory milieu within the tumor microenvironment can be hijacked to potentiate malignant phenotypes. Such insights could hold translational value beyond breast cancer, particularly in other malignancies where adipocyte-rich niches and inflammatory cytokines play pivotal roles.
Furthermore, the study brings to light the intricate feedback loops that maintain cancer cell plasticity and stemness. By sustaining STAT3 and NF-κB activation, the IL6-CXCL1 axis likely contributes to the epithelial-to-mesenchymal transition (EMT), a process essential for metastatic competency. This molecular crosstalk hence not only supports local tumor growth but may also facilitate distant organ colonization, a hallmark of TNBC’s aggressive clinical course.
The translational implications also extend to immunotherapy strategies. Since both STAT3 and NF-κB regulate genes involved in immune evasion, the IL6/CXCL1-dependent microenvironment could create an immunosuppressive niche, blunting anti-tumor immune responses. Combining inhibitors that disrupt this axis with immune checkpoint blockade could therefore enhance therapeutic efficacy in TNBC, an area currently under intense investigation.
One of the study’s strengths lies in the integration of in vitro analyses with in vivo modeling and patient-derived data, which collectively strengthen the translational applicability of the conclusions. The authors convincingly demonstrate that modulating the IL6/CXCL1-STAT3/NF-κB pathways significantly alters tumor growth and metastatic potential in experimental models, bolstering the foundation for clinical translation.
Looking forward, the research team proposes further exploration into the heterogeneity of adipocyte populations within the breast tumor microenvironment and their differential secretome profiles. Understanding how various adipocyte subsets contribute to IL6 production and their interactions with cancer cells could refine therapeutic targeting strategies. Additionally, investigating the temporal dynamics of this crosstalk during tumor evolution and in response to therapy could reveal critical windows for intervention.
In sum, this seminal work uncovers a finely tuned cytokine network that bridges adipocytes and triple-negative breast cancer cells, orchestrating a potent activation of oncogenic pathways that drive tumor progression. By revealing the concerted role of IL6 and CXCL1 in co-activating the STAT3/NF-κB axis, Ruan and colleagues provide a compelling rationale for targeting tumor-microenvironment interactions in the ongoing battle against one of the most aggressive forms of breast cancer.
Subject of Research:
The molecular crosstalk between adipocytes and triple-negative breast cancer cells mediated by IL6 and CXCL1 and its activation of the STAT3/NF-κB signaling pathways.
Article Title:
Adipocyte-derived IL6 and triple-negative breast cancer cell-derived CXCL1 co-activate STAT3/NF-κB pathway to mediate the crosstalk between adipocytes and triple-negative breast cancer cells.
Article References:
Ruan, GT., Zhu, LC., Xie, HL. et al. Adipocyte-derived IL6 and triple-negative breast cancer cell-derived CXCL1 co-activate STAT3/NF-κB pathway to mediate the crosstalk between adipocytes and triple-negative breast cancer cells. Cell Death Discov. 11, 395 (2025). https://doi.org/10.1038/s41420-025-02713-4
Image Credits:
AI Generated
DOI:
https://doi.org/10.1038/s41420-025-02713-4
Tags: adipocyte interleukin 6 role in canceradipocyte-cancer cell crosstalkadipocytes and cancer cell communicationbreast tissue fat cells in cancerCXCL1 chemokine in cancercytokines in tumor aggressionmalignant behavior of TNBCmetabolic reprogramming in cancer cellsSTAT3 NF-κB signaling pathwaystriple-negative breast cancer mechanismstumor microenvironment interactionstumor progression and therapeutic resistance