In a groundbreaking longitudinal study spanning half a decade, scientists have unveiled significant shifts in the susceptibility of Plasmodium falciparum—the deadliest malaria parasite species—to commonly used antimalarial drugs across Uganda. This research, covering the years 2019 to 2024, provides critical insights into the evolving landscape of malaria treatment efficacy in a region disproportionately burdened by the disease. The study’s comprehensive data reveal complex patterns of drug resistance, which could profoundly influence future malaria control and eradication strategies on the African continent and beyond.
Malaria remains a global health menace, with approximately 200 million cases reported annually, and P. falciparum is responsible for the majority of severe illness and fatalities. Antimalarial drugs, especially artemisinin-based combination therapies (ACTs), have formed the cornerstone of malaria treatment in endemic countries like Uganda. However, the rise of drug-resistant parasite strains threatens to undermine these gains. This investigation meticulously tracked changes in parasite susceptibility, focusing on molecular markers linked to resistance, clinical treatment outcomes, and genetic diversity among parasite populations over the course of five years.
The study utilized a robust surveillance framework encompassing both molecular and phenotypic assessments of P. falciparum isolates collected from sentinel sites across Uganda. High-throughput sequencing technologies facilitated detailed genotyping of key resistance genes, including pfkelch13—a gene widely known to confer artemisinin resistance—and pfcrt, associated with chloroquine resistance. Additionally, in vitro drug sensitivity assays measured the parasites’ growth inhibition in response to a spectrum of antimalarial compounds, providing functional corroboration to genetic findings.
.adsslot_qmYfsPDSC7{ width:728px !important; height:90px !important; }
@media (max-width:1199px) { .adsslot_qmYfsPDSC7{ width:468px !important; height:60px !important; } }
@media (max-width:767px) { .adsslot_qmYfsPDSC7{ width:320px !important; height:50px !important; } }
ADVERTISEMENT
One of the pivotal findings from 2019 to 2024 was an incremental increase in mutations linked to partial artemisinin resistance. This subtle yet concerning trend signals that despite the continued efficacy of ACTs in most regions, P. falciparum is gradually adapting under therapeutic pressure. Notably, mutations in the pfkelch13 gene rose from a baseline frequency of under 2% in 2019 to approximately 7% by 2024, a statistically significant change indicative of an emerging resistance phenotype. While these mutations do not yet translate to widespread treatment failure, they necessitate vigilant monitoring to preempt the establishment of fully resistant parasite populations.
Equally critical were the observations regarding partner drug susceptibility within ACT regimens. Declines in sensitivity to lumefantrine and piperaquine were detected, raising alarms about the durability of current first-line therapies. The study attributes these trends to selective pressures exerted by widespread drug use, which may inadvertently favor resistant clones. This underscores the urgency for periodic drug efficacy assessments and, potentially, the preemptive introduction of novel antimalarials or combination therapies to outpace resistance evolution.
Beyond resistance markers, the researchers documented shifts in the P. falciparum population structure. Genetic diversity analyses revealed a modest reduction in overall heterogeneity, suggesting a possible bottleneck effect driven by sustained control measures and drug pressure. Such population dynamics are crucial, as they influence the parasite’s capacity to adapt and may reflect localized success in transmission reduction. However, pockets of high genetic diversity persisted, especially in regions with inconsistent healthcare access, illuminating persistent challenges in achieving uniform malaria control.
The implications of this research extend to public health policy and malaria management. The gradual erosion of drug susceptibility in Uganda signals the need for dynamic therapeutic guidelines that adapt to evolving resistance patterns. The study advocates for integrating resistance marker surveillance into routine malaria monitoring programs, enabling real-time data-driven decisions. Furthermore, the authors emphasize strengthening community-based interventions to mitigate transmission hotspots that act as reservoirs for resistant parasites.
Crucially, this research exemplifies the power of collaborative, multidisciplinary approaches in tackling malaria. It combined epidemiological data, molecular biology, and clinical insights from government health agencies, academic institutions, and frontline healthcare workers. Such integrated efforts are paramount in constructing a detailed, actionable picture of resistance trends and their impact on treatment efficacy.
In addition to surveillance, the study promotes the acceleration of antimalarial drug development pipelines. Resistance to currently deployed compounds, even if still emergent, threatens to reverse decades of progress. Investment in novel classes of antimalarials that bypass known resistance mechanisms or target different parasite life cycle stages is imperative. The research team highlights promising candidates in early clinical trials, but warns that their widespread deployment must be coupled with robust stewardship to preserve their efficacy.
The findings also spotlight the role of genomic technologies in infectious disease control. Advanced sequencing and bioinformatics enabled high-resolution tracking of resistance mutations and parasite population changes over time. This technological prowess empowers researchers and public health officials to anticipate resistance trajectories and implement preemptive measures—a paradigm shift from reactive to proactive malaria management.
Moreover, the study’s geographic focus on Uganda offers valuable lessons for other malaria-endemic regions. Uganda’s diverse epidemiological landscape, ranging from high-transmission rural areas to urban centers with variable health infrastructure, provides a microcosm for understanding resistance dynamics in sub-Saharan Africa. Insights gained here can inform tailored interventions elsewhere, recognizing that one-size-fits-all approaches may falter amid local diversity.
The research also addresses the social and economic dimensions influencing resistance emergence. It acknowledges that inconsistent drug quality, substandard dosing, and self-medication practices contribute to selective pressures that drive resistance. Strengthening pharmaceutical regulation and community education is therefore integral to comprehensive resistance mitigation strategies.
Furthermore, the study underscores the importance of sustained funding in malaria control research. Longitudinal, high-resolution datasets are expensive and logistically challenging to maintain but essential for capturing the nuanced evolution of parasite susceptibility. The authors call on global health agencies and donors to prioritize continuous surveillance frameworks rather than episodic investigations.
Finally, the emerging data from 2019 to 2024 offer a cautiously optimistic narrative. Although resistance markers have increased, current ACTs largely remain efficacious, and intensified control measures appear to suppress transmission intensity in several regions. This window of opportunity should galvanize intensified efforts to preempt resistance-driven treatment failures and sustain the momentum towards malaria elimination.
In conclusion, this landmark study illuminates the shifting battleground in Uganda’s fight against malaria, revealing early warning signs of drug resistance evolution in Plasmodium falciparum. Its nuanced insights into genetic, phenotypic, and epidemiological changes underscore the complexity of managing antimalarial drug efficacy in real-world settings. The research serves as both a scientific beacon and a clarion call for adaptive, integrated strategies combining surveillance, drug development, policy reform, and community engagement to sustain and accelerate malaria control achievements globally.
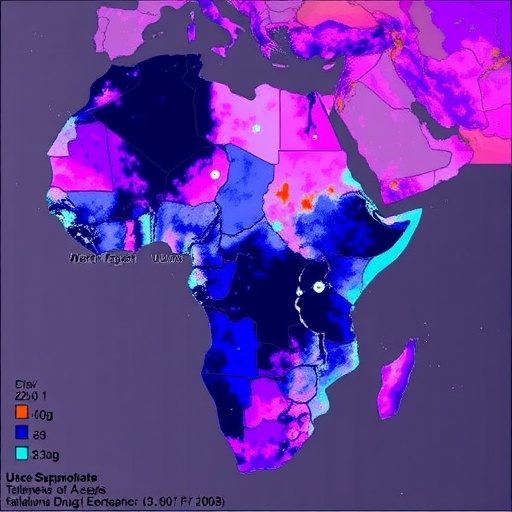
Subject of Research: Changes in susceptibility of Plasmodium falciparum to antimalarial drugs over time in Uganda.
Article Title: Changes in susceptibility of Plasmodium falciparum to antimalarial drugs in Uganda over time: 2019–2024.
Article References:
Okitwi, M., Orena, S., Tumwebaze, P.K. et al. Changes in susceptibility of Plasmodium falciparum to antimalarial drugs in Uganda over time: 2019–2024. Nat Commun 16, 7353 (2025). https://doi.org/10.1038/s41467-025-62810-x
Image Credits: AI Generated
Tags: antimalarial drug resistance patternsartemisinin-based combination therapiesdrug susceptibility monitoring Ugandaevolving malaria treatment strategiesgenetic diversity of malaria parasitesglobal health challenges malarialongitudinal study on malariamalaria control and eradication effortsmalaria surveillance and genotypingmalaria treatment efficacy Ugandamolecular markers of drug resistancePlasmodium falciparum drug resistance