In the evolving landscape of forensic radiology, postmortem imaging techniques continue to revolutionize the approach to pediatric autopsies, expanding the capabilities of medico-legal investigations. A groundbreaking systematic review recently published by Vanhaebost and colleagues has delved into the utility of postmortem computed tomography angiography (PMCTA) specifically tailored for fetuses, infants, and children up to twelve years old. This comprehensive study sheds new light on the technical intricacies, challenges, and viable protocols for imaging small bodies, offering invaluable guidance that may ultimately redefine pediatric postmortem examinations.
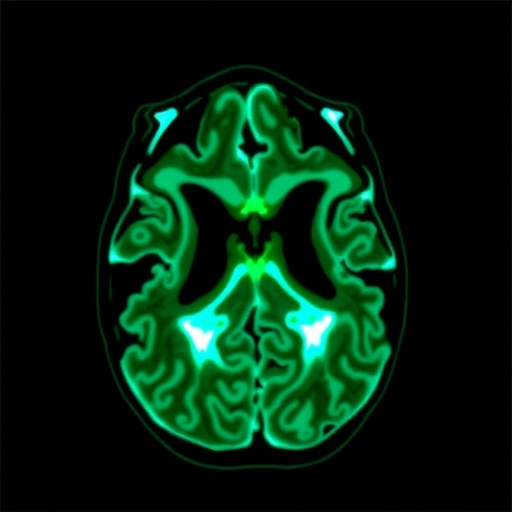
Postmortem CT angiography is an advanced imaging technique that enables detailed visualization of the vascular system after death through the injection of radiopaque contrast agents. While extensively utilized in adult forensic investigations, its application in pediatric cases has been limited due to anatomical, technical, and procedural complexities. The reviewed study systematically compiles existing evidence on PMCTA in younger populations and addresses an important knowledge gap by proposing a conceptual decision tree to guide forensic practitioners in clinical and legal scenarios involving minors.
The unique challenges inherent to performing PMCTA on fetuses and young children stem from their size, fragility, and the often delicate state of postmortem tissues. Traditional autopsy has long been regarded as the gold standard, yet it can be invasive and understandably distressing for grieving families. Radiological alternatives such as PMCTA provide a less intrusive avenue to ascertain causes of death, detect vascular anomalies, and identify potential trauma or pathological conditions, thus enhancing diagnostic accuracy without compromising respect for the deceased.
.adsslot_06FGyOQzkl{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_06FGyOQzkl{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_06FGyOQzkl{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
Technically, performing PMCTA in this demographic demands careful consideration of injection methods, contrast preparation, and imaging parameters. The vascular calibers in fetuses and infants are minuscule relative to adults, requiring innovative catheterization techniques and highly specialized contrast media tailored to ensure adequate perfusion while avoiding extravasation and artifact generation. The authors in the review contrast diverse protocols and highlight the importance of customizing approaches according to age group, cause of death suspicion, and available institutional resources.
Another critical aspect emerging from this systematic review is the distinction between angiographic protocols that employ invasive versus non-invasive access to the cardiovascular system. Some studies rely on cannulation of large vessels such as the umbilical artery or vein in fetuses, while others utilize direct cardiac puncture. The variations in contrast agent viscosity and injection pressures also play pivotal roles in achieving satisfactory vascular opacification, which is essential for rendering high-definition images capable of elucidating subtle pathological findings that might otherwise remain obscured.
One of the key contributions of this work is the development of a conceptual decision tree, an evidence-based framework designed to assist forensic radiologists and pathologists in selecting the appropriate PMCTA modality. The decision algorithm integrates factors such as the age and size of the deceased, the suspected pathology, time since death, and equipment availability. Its implementation aims at standardizing workflows, reducing procedural errors, and optimizing diagnostic yield, ultimately supporting judicial processes through more precise cause-of-death determinations.
Importantly, the study highlights the diagnostic potential of PMCTA to detect cardiovascular malformations, thromboembolic events, and traumatic injuries that might be missed or inadequately characterized by conventional autopsy alone. In perinatal medicine, where fetal demise etiology often entails complex vascular components, non-invasive angiography can offer unprecedented insights into in utero vascular physiology and pathology, bridging gaps in medical knowledge and legal evidence.
Nevertheless, the authors caution against overreliance on imaging, emphasizing that PMCTA should complement rather than replace traditional autopsy methods. Limitations such as constrained resolution in extremely small vessels, difficulties in postmortem redistribution of contrast, and operator dependency necessitate a multidisciplinary approach. Collaborative interpretation involving forensic pathologists, radiologists, and pediatric specialists remains paramount to ensure accurate, holistic case evaluations.
The ethical dimensions surrounding postmortem imaging in children also feature prominently in the discussion. Minimally invasive techniques like PMCTA align with parents’ preferences for less disruptive postmortem investigations and reduce the psychological burden associated with full autopsy. These technological advances may foster higher autopsy consent rates, vital for advancing medical and forensic sciences, preventing future tragedies, and informing public health policies.
Furthermore, the review underscores the importance of standardized training and credentialing for forensic professionals embracing PMCTA. Given the technical nuances and potential diagnostic pitfalls, establishing rigorous educational programs and inter-institutional quality control measures is crucial to guarantee consistency, accuracy, and legal defensibility of imaging findings.
The integration of artificial intelligence and machine learning for image reconstruction and automated anomaly detection emerges as a promising frontier referenced in the systematic analysis. By harnessing these computational tools, forensic radiologists can potentially accelerate image interpretation, uncover subtle vascular abnormalities, and generate reproducible diagnostic outputs, paving the way towards scalable implementation of pediatric PMCTA worldwide.
Moreover, the authors advocate for international collaborations to harmonize imaging protocols and consolidate multicentric datasets, ensuring that pediatric PMCTA benefits from broader validation and technological refinement. Such initiatives would enable robust meta-analytical studies, improve diagnostic algorithms, and facilitate regulatory approvals of specialized contrast agents designed for pediatric postmortem angiography.
This comprehensive review by Vanhaebost et al. represents a significant advancement in forensic imaging scholarship. By meticulously analyzing current evidence, documenting technical challenges, and proposing a rational decision-making model, it lays the groundwork for PMCTA to become a cornerstone in pediatric forensic investigations. Adoption of these recommendations promises to enhance diagnostic accuracy, respect cultural sensitivities, and accelerate judicial resolutions in cases involving the youngest and most vulnerable deceased.
Ultimately, as forensic science embraces ever more sophisticated imaging modalities, the interface between technology, medicine, and law continues to evolve. Postmortem CT angiography for fetuses and children epitomizes this trend, offering a powerful, non-invasive window into the silent final chapters of life. The ongoing refinement and dissemination of such innovative methods will no doubt transform the landscape of postmortem diagnostics and elevate standards of care for forensic investigations across the globe.
Subject of Research: Forensic applications of postmortem CT angiography in fetuses, infants, and children up to 12 years old.
Article Title: Postmortem CT angiography of fetuses, infants and children up to 12 years old: a systematic review and conceptual decision tree.
Article References:
Vanhaebost, J., Scholzen, T., Coche, E. et al. Postmortem CT angiography of fetuses, infants and children up to 12 years old a systematic review and conceptual decision tree. Int J Legal Med (2025). https://doi.org/10.1007/s00414-025-03556-5
Image Credits: AI Generated
Tags: challenges in pediatric imagingdecision tree for forensic practitionersforensic investigations in minorsforensic radiology advancementsimaging protocols for small bodiesmedico-legal implications of PMCTApediatric autopsiespostmortem computed tomography angiographypostmortem imaging techniquessystematic review of PMCTAtechnical intricacies of pediatric postmortem examinationsvascular visualization after death