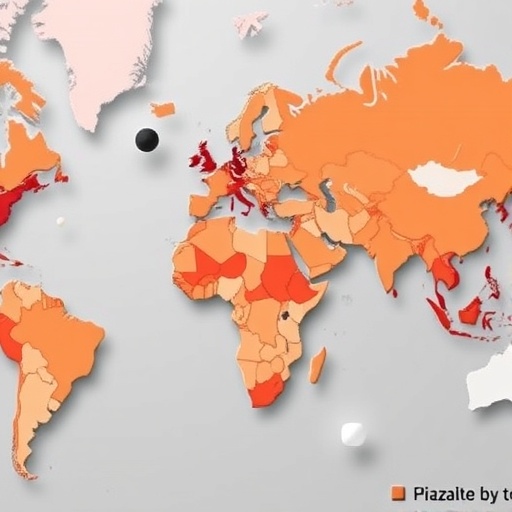
In the rapidly evolving landscape of global health, diabetes remains one of the most formidable challenges facing low- and middle-income countries (LMICs). A groundbreaking study recently published in Nature Communications provides an unprecedented national-level overview of the utilization patterns of glucose-lowering medications across 62 LMICs. This extensive research offers critical insights into the accessibility, affordability, and diversity of diabetes treatment in settings where healthcare infrastructure is often constrained. By harnessing data drawn from national health surveys and pharmaceutical databases, the researchers paint a detailed portrait of how LMICs confront the complex burden of diabetes management through medical therapy.
At the heart of the investigation lies the question of how diabetes medications are being used in countries where economic and systemic limitations can hinder optimal care. In stark contrast to high-income nations, LMICs face a plethora of barriers including inconsistent drug supply chains, financial inaccessibility, and insufficient healthcare worker training. These factors collectively influence the types of glucose-lowering agents prescribed and consumed by patients. The study’s meticulous compilation and analysis of nationally representative data sets illuminate pivotal disparities not only in the availability of essential medications but also in the therapeutic approaches adopted within these diverse populations.
The study highlights how metformin, a first-line therapy internationally recommended for type 2 diabetes, is the most widely used glucose-lowering agent across the surveyed countries. Its relatively low cost, extensive clinical experience, and efficacy have made it a staple in diabetes treatment protocols globally. However, the research uncovers significant heterogeneity in metformin’s penetration in LMICs, signaling persistent barriers to universal access. Some nations reveal near-universal availability in public health facilities, while others reflect alarming gaps, underscoring how economic stratification and health policy directly affect medication distribution.
.adsslot_G0LhwtKVrH{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_G0LhwtKVrH{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_G0LhwtKVrH{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
Beyond metformin, the research delves deeply into the prevalence of sulfonylureas, DPP-4 inhibitors, and insulin use, each illustrating different narratives of access and application. Sulfonylureas, owing to their affordability and longstanding history, are frequently employed despite their less favorable side effect profiles compared to newer drugs. Notably, the use of DPP-4 inhibitors and other modern agents is far less common in the studied countries, primarily because of their higher costs and limited inclusion in national formularies. Insulin usage presents a particularly complex scenario, reflecting dire challenges in delivery and storage, given its necessity for many patients but requirement for cold chain maintenance.
Intriguingly, the study’s geographic juxtaposition reveals stark contrasts not only between countries but also within regions. For instance, in parts of Sub-Saharan Africa and South Asia, significant strides have been made in expanding access to essential oral medications, whereas some nations remain entrenched in antiquated treatment paradigms or face critical medication shortages. These findings vividly illustrate the uneven landscape of diabetes care, highlighting the urgency for targeted interventions that reconcile local realities with global treatment standards.
The implications of these disparities transcend pharmacological considerations. The authors underscore that inadequate access to glucose-lowering medications contributes substantially to poor glycemic control and heightened rates of diabetes complications, including cardiovascular disease, kidney failure, and neuropathy. This ripple effect imposes a catastrophic toll on the already overstretched health systems of LMICs and amplifies socioeconomic inequalities. By providing robust national data, the study empowers policymakers and global health advocates to tailor diabetes care strategies more effectively, ensuring that therapeutic advances and guidelines translate into real-world improvements.
Methodologically, the research stands out for its rigorous approach combining multiple data modalities, such as household surveys capturing self-reported medication use alongside health facility assessments documenting drug availability. This multifaceted approach mitigates common biases and strengthens confidence in the findings. Moreover, by encompassing a vast number of countries across continents, the study circumvents the common pitfall of localized data that may not be generalizable. Consequently, its conclusions are poised to inform both regional and global frameworks for diabetes care.
Another revelation from the study pertains to the policy environment governing diabetes treatment in LMICs. While international guidelines promote stepwise intensification of therapy based on patient needs, the reality in many surveyed countries is constrained by formularies that exclude newer, more effective, but costlier agents. This disconnect is exacerbated by inconsistent training among healthcare workers, limiting their comfort in prescribing complex regimens or insulin. The study thereby underscores the critical need for capacity building initiatives and policy reforms that expand the armamentarium available to clinicians treating diabetes.
Technology and innovation also emerge as critical factors in the future trajectory of diabetes management in LMICs. As digital health solutions proliferate, especially in telemedicine and mobile health, they hold potential to bridge gaps in education, adherence monitoring, and timely medication titration. However, the present study stops short of evaluating these aspects, focusing instead on the foundational issue of drug availability. Nevertheless, the findings create a vital evidence base that can be leveraged to integrate innovative approaches with core access improvements, potentially revolutionizing care delivery.
The economic implications woven throughout the study merit close attention. The cost barriers faced by patients in LMICs are formidable, leading to medication non-adherence and treatment discontinuation. The research illuminates how pooled procurement mechanisms or subsidized programs could alleviate these burdens, drawing on successful models from immunization and HIV care. Such strategies could lower prices and stabilize supplies, making life-saving glucose-lowering drugs truly affordable. The study thereby catalyzes a necessary dialogue on sustainable financing in the diabetes domain.
Importantly, the research also frames diabetes care within the broader context of non-communicable disease (NCD) management in LMICs. Given that many countries grapple simultaneously with infectious diseases and a growing NCD burden, diabetes treatment competes for limited resources. The insights generated here provide a compelling argument for integrated, health system strengthening approaches that synergistically address multiple chronic conditions rather than episodic, disease-specific interventions.
From a clinical research perspective, the study prompts new questions regarding treatment outcomes linked to observed medication patterns. Does reduced access to newer agents correlate with poorer clinical endpoints? How do local cultural beliefs and health literacy impact adherence and effective use? While the current work lays the groundwork, future longitudinal studies correlating medication use with patient-level outcomes will be essential to fully understand the impact of therapeutic availability in LMICs.
This seminal research represents a clarion call to all stakeholders involved in diabetes care—from governments to non-governmental organizations, pharmaceutical companies, and global health bodies. The documented gaps and disparities are not mere statistics but signify millions of lives compromised by suboptimal treatment. Bridging these divides requires coordinated action that harmonizes policy reform, financing, healthcare workforce development, and community engagement.
As the global diabetes epidemic intensifies, particularly in the world’s most vulnerable regions, this study’s comprehensive assessment provides both a benchmarking tool and a roadmap. Sharpening focus on equitable access to glucose-lowering medications must become a global health priority, anchoring sustainable progress in diabetes outcomes for millions. The findings compel us to rethink and reimagine diabetes care paradigms in LMICs—not as isolated challenges but integral to global health equity.
In conclusion, this extensive national-level examination of glucose-lowering medication usage across 62 LMICs is an influential milestone in diabetes research. By illuminating patterns of medication use and availability, the study identifies critical gaps that hinder effective diabetes management. Its implications resonate far beyond the pages of scientific literature, touching the lives of millions worldwide who battle diabetes daily. The research offers a beacon of data-driven hope, guiding future interventions toward more accessible, affordable, and effective diabetes treatments across the globe.
Subject of Research: National-level patterns and disparities in glucose-lowering medication use for diabetes management in low- and middle-income countries.
Article Title: National evidence on glucose-lowering medication use for diabetes from 62 low- and middle-income countries.
Article References:
Teufel, F., Roddewig, P., Marcus, M.E. et al. National evidence on glucose-lowering medication use for diabetes from 62 low- and middle-income countries. Nat Commun 16, 7139 (2025). https://doi.org/10.1038/s41467-025-59123-4
Image Credits: AI Generated
Tags: barriers to diabetes care in developing nationsdiabetes medication supply chain issuesdiabetes medication usage in low-income countriesdiabetes treatment affordability in LMICsdisparities in diabetes management practicesfinancial barriers to diabetes treatmentglucose-lowering medications accessibilityhealthcare infrastructure in low- and middle-income countriesmetformin utilization in global healthnational health surveys on diabetespharmaceutical databases for diabetes researchtraining needs for healthcare workers in LMICs