In a groundbreaking study published in Nature Communications, researchers have unveiled a pivotal role of CD142-positive synovial fibroblasts in the progression of meniscus destruction within the inflammatory landscape of rheumatoid arthritis (RA). This discovery sheds light on the cellular mechanisms underlying joint degradation and opens new avenues for targeted therapeutic interventions aimed at preserving joint integrity in RA patients.
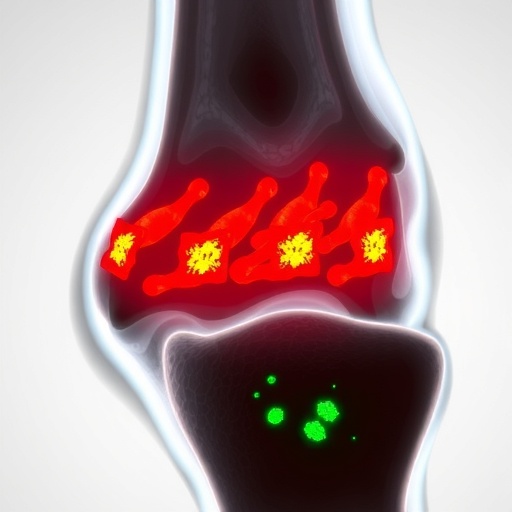
Rheumatoid arthritis, a chronic autoimmune disease, is notorious for causing persistent inflammation and progressive joint damage. The meniscus, a fibrocartilaginous structure crucial for load distribution and joint stability in the knee, often suffers irreversible degeneration in RA, exacerbating pain and disability. Despite extensive studies on immune cell contributions, the specific stromal cell subtypes orchestrating meniscal damage remained elusive until now.
The research team, led by Sun, H., Lin, X., Liu, F. and colleagues, leveraged advanced single-cell transcriptomic analyses to delineate the heterogeneity of synovial fibroblasts within RA-affected joints. Synovial fibroblasts, the resident connective tissue cells lining the joint capsule, have long been implicated in joint inflammation, but their precise roles in meniscal integrity and pathological destruction were poorly defined. Their findings identified a CD142-positive subset of synovial fibroblasts that emerge prominently during RA progression.
.adsslot_KiOweJVo29{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_KiOweJVo29{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_KiOweJVo29{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
CD142, also known as tissue factor, is a transmembrane glycoprotein recognized predominantly for its role in the initiation of coagulation cascades. However, this study expands its significance beyond hematologic functions, implicating CD142 expression as a marker of a highly destructive fibroblast phenotype within inflamed synovial tissue. These specialized fibroblasts exhibit a pro-inflammatory and matrix-degrading secretome, characterized by elevated expression of cytokines, chemokines, and matrix metalloproteinases.
Functionally, CD142-positive synovial fibroblasts were shown to directly interact with meniscal cells and extracellular matrix components, mediating degradation and architectural disassembly. Through ex vivo organ culture systems, the authors demonstrated that conditioned media from CD142-positive fibroblasts induced significant meniscal cartilage breakdown, mimicking the pathology observed in RA patients. This catabolic effect was not observed with conditioned media from CD142-negative fibroblast populations, underscoring the pathogenic specificity of the CD142-positive subset.
Furthermore, in vivo murine models of inflammatory arthritis recapitulated the expansion of CD142-expressing fibroblasts concomitant with meniscal erosion, reinforcing the pathological relevance across species. Genetic ablation or pharmacological inhibition of CD142 signaling pathways attenuated fibroblast-driven meniscal damage, suggesting promising therapeutic potential. Such interventions could preserve meniscal structure, thereby maintaining joint functionality and ameliorating clinical symptoms.
Beyond matrix degradation, the study uncovered that CD142-positive synovial fibroblasts contribute to the amplification of local inflammatory networks. These cells secrete chemotactic factors that recruit immune effector cells, including macrophages and T cells, creating a feedback loop that sustains synovitis and joint destruction. This dual role as both effectors of tissue damage and facilitators of immune cell infiltration positions CD142-positive fibroblasts as central orchestrators of RA pathogenesis.
The molecular mechanisms governing the differentiation and activation of CD142-positive fibroblasts were partially elucidated in the study. Key signaling pathways, notably those involving transforming growth factor-beta (TGF-β) and nuclear factor kappa B (NF-κB), modulate CD142 expression and fibroblast phenotypic switching. These pathways represent viable targets for pharmacological modulation aimed at disrupting the fibroblast-mediated tissue destruction axis.
Importantly, the identification of CD142 as a surface marker enables potential diagnostic advancements. Using flow cytometry and immunohistochemical techniques, clinicians could quantify CD142-positive fibroblast abundance as a biomarker of disease severity and progression. This stratification tool could facilitate personalized treatment plans, optimizing therapeutic outcomes for RA patients.
The translational implications of this study are profound. Current therapeutic regimens for RA primarily focus on systemic immunosuppression, which may limit inflammatory damage but often fail to fully prevent joint structural deterioration. Targeting pathological fibroblast subsets like CD142-positive cells introduces a complementary strategy that directly addresses tissue destruction rather than only modulating inflammation.
Moreover, this fibroblast-focused approach might avoid some of the adverse effects linked to generalized immunosuppression, such as increased vulnerability to infections. By specifically inhibiting detrimental synovial fibroblast functions, patient safety profiles of future treatments may improve, alongside clinical efficacy.
This research aligns with a growing paradigm shift in rheumatology, emphasizing the microenvironment and stromal components as key players rather than solely the immune system. The synovial fibroblast, once considered a passive participant, is now recognized as an active driver of pathology. Understanding this complex cellular crosstalk rewrites the narrative of joint destruction and opens doors for novel biomarkers and drug targets.
Future directions stemming from these findings include the development of monoclonal antibodies or small molecules that selectively bind CD142 or its downstream signaling mediators. Clinical trials assessing the safety and effectiveness of such agents will be crucial. Additionally, integrating this knowledge with existing therapies might yield synergistic effects, enhancing comprehensive disease management.
In summary, the identification of CD142-positive synovial fibroblasts as key mediators of meniscus destruction revolutionizes our understanding of rheumatoid arthritis pathogenesis. This discovery not only elucidates the cellular drivers of joint degradation but also offers tangible prospects for innovative therapeutic strategies aimed at preserving joint integrity and improving patient quality of life. As the field moves forward, harnessing the pathogenic potential of these fibroblast subsets could redefine standards of care in RA.
Subject of Research: The role of CD142-positive synovial fibroblasts in meniscus destruction within rheumatoid arthritis.
Article Title: CD142-positive synovial fibroblasts drive meniscus destruction in rheumatoid arthritis.
Article References:
Sun, H., Lin, X., Liu, F. et al. CD142-positive synovial fibroblasts drive meniscus destruction in rheumatoid arthritis. Nat Commun 16, 6942 (2025). https://doi.org/10.1038/s41467-025-61842-7
Image Credits: AI Generated
Tags: advanced cellular research in arthritisCD142-positive synovial fibroblastschronic autoimmune disease impactsfibrocartilage degeneration in RAinflammatory joint diseasesjoint degradation mechanismsmeniscal integrity preservationrheumatoid arthritis meniscus damagesingle-cell transcriptomic analysissynovial fibroblasts in joint inflammationtargeted therapies for RAtissue factor in synovial cells