A recent randomized controlled trial conducted in Germany has shed light on an innovative approach to addressing post-traumatic stress disorder (PTSD) among survivors of critical illness discharged from intensive care units (ICU). Published in The BMJ, the study investigates the impact of a brief, general practitioner-led narrative exposure intervention designed to reduce PTSD symptoms in a primary care setting. This intervention, while modest in effect, offers promising insights into bridging the gap between acute medical care and specialized mental health services, particularly in healthcare systems constrained by limited resources and long wait times for psychiatric treatment.
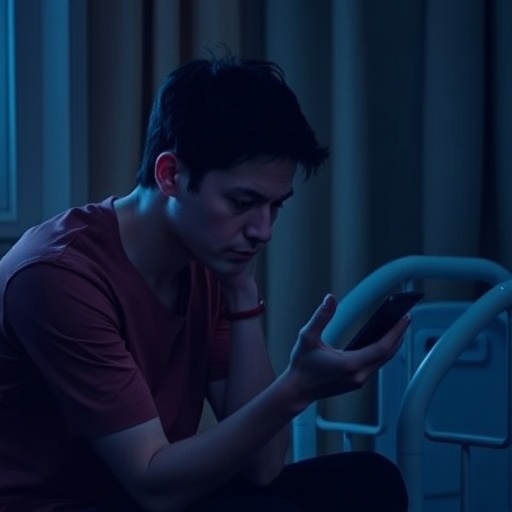
Post-traumatic stress disorder is a common and debilitating consequence faced by approximately 20% of ICU survivors. The experience of critical illness and the often traumatic nature of intensive care treatments contribute to severe psychological distress. Despite its prevalence, existing primary care frameworks have largely lacked structured, evidence-based interventions tailored to PTSD symptoms within this population. This gap in aftercare amplifies the risk of chronic psychiatric morbidity and hampers overall recovery and quality of life.
The German research team addressed this unmet clinical need by designing a multicenter, observer-blinded, randomized controlled trial involving 319 adult patients drawn from general practice clinics across the country. Participants, with an average age of 58 years and a predominance of males (61%), were randomized to receive either a targeted psychological intervention or an improved standard of care. The intervention consisted of three structured consultations with general practitioners trained briefly in narrative exposure therapy, supplemented by eight follow-up interactions with nursing staff focusing on PTSD symptomatology.
Narrative exposure therapy, rooted in trauma-focused cognitive-behavioral approaches, enables patients to systematically recount and process traumatic memories within a supportive therapeutic environment. This method was adapted for feasibility in general practice, emphasizing brevity and integration into routine post-ICU care. The control group continued to receive usual care, albeit with enhancements to reflect contemporary standards of general practice aftercare for critically ill patients.
The principal outcome was the severity of PTSD symptoms at six months post-intervention, quantified using the well-validated post-traumatic diagnostic scale (PDS-5). This instrument assigns scores ranging from 0 to 80, with higher values indicating greater symptom severity. The trial’s prespecified minimal clinically important difference (MCID) was established at six points, marking the threshold for a meaningful therapeutic effect.
Baseline PDS-5 scores averaged 30.6 in both groups, demonstrating moderate PTSD symptom burden prior to intervention. At six months, the intervention group exhibited a mean reduction of 6.2 points, whereas the control group showed a decrease of 1.5 points, culminating in an adjusted difference of 4.7 points. Although this difference did not meet the MCID, it indicated a trend toward symptom improvement attributable to the narrative exposure therapy. By 12 months, the intervention cohort sustained and slightly enhanced this benefit, with a 7.9-point reduction compared to 2.5 points in controls, resulting in a 5.4-point difference, still below the MCID threshold.
Several factors potentially explain the modest magnitude of symptom reduction observed. The intervention’s brevity and low intensity likely limited its therapeutic potency, particularly in a population with diverse and complex PTSD presentations. Additionally, patients with severe PTSD symptoms were excluded from the study, historically a subgroup demonstrating the greatest potential for improvement with intensive psychotherapies. Moreover, the relatively brief and pragmatic training provided to general practitioners may have constrained the fidelity and depth of the narrative exposure delivery.
Despite these limitations, the trial importantly demonstrated the feasibility of embedding trauma-focused psychological interventions within the primary care setting, a critical consideration for health systems where specialist mental health services are scarce or burdened by long waitlists. The findings corroborate the hypothesis that early, low-threshold psychological support may mitigate the psychological sequelae of critical illness, thereby improving patient outcomes in a cost-effective and accessible manner.
Beyond PTSD symptomatology, researchers noted improvements in secondary outcomes encompassing depressive symptoms, functional disability, and quality of life metrics. These broader benefits reinforce the interconnectedness of mental health with overall well-being and underscore the value of integrated aftercare strategies following ICU discharge. Such effects further justify continued exploration of GP-led interventions as adjuncts to conventional psychiatric care.
The investigative team conceded the possibility of confounding variables influencing results, given the absence of blinding among participating practitioners and patients, as well as the complexity of post-ICU psychological trajectories. They advocate for future research to refine the content and delivery mechanisms of such interventions, emphasizing scalability, therapeutic intensity, and patient selection criteria to optimize efficacy.
Complementing the main study, a linked editorial published alongside the trial contextualizes the intervention as a significant stride toward trauma-informed primary care. The editorial highlights the pragmatic advantages of early narrative exposure therapy in facilitating psychological recovery when specialist resources are limited, while simultaneously cautioning against interpreting this model as a substitute for comprehensive psychiatric treatment.
The study and accompanying commentary together signal a paradigm shift in post-critical illness care, emphasizing the necessity of bridging acute medical services with longitudinal psychological support through general practice. Advancements in this domain have profound implications for patient trajectories, potentially attenuating the long-term mental health burden associated with surviving catastrophic medical events.
In summary, the German multicenter trial offers compelling evidence supporting the integration of brief, GP-led narrative exposure therapy within primary care settings to address the unmet need for early PTSD intervention among ICU survivors. Although the clinical effect sizes were below predefined thresholds, the approach demonstrates considerable promise as a scalable, resource-sensitive strategy to alleviate psychological distress and enhance recovery outcomes. Future research will be essential to optimize intervention parameters, training protocols, and systemic implementation, ultimately aiming to transform the landscape of post-ICU mental health care on a global scale.
Subject of Research: People
Article Title: Research: Effects of a general practitioner-led brief narrative exposure intervention on symptoms of post-traumatic stress disorder after care in an intensive care unit (PICTURE): multicentre, observer blind, randomised controlled trial
News Publication Date: 7-May-2025
Web References: http://dx.doi.org/10.1136/bmj-2024-082092
Keywords: Post traumatic stress disorder
Tags: bridging medical care and mental healthchronic psychiatric morbiditycritical illness psychological impactevidence-based interventions for PTSDGP-led therapy for PTSDimproving recovery after critical illnessmental health services accessibilitynarrative exposure interventionprimary care mental healthPTSD in ICU survivorsPTSD treatment in primary carerandomized controlled trial Germany