Singapore, 27 June 2024 – Researchers from the Critical Analytics for Manufacturing Personalized-Medicine (CAMP) Interdisciplinary Research Group (IRG) at Singapore-MIT Alliance for Research and Technology (SMART), MIT’s research enterprise in Singapore, have developed a novel method capable of producing clinical doses of viable autologous chimeric antigen receptor (CAR) T-cells in a ultra-small automated closed-system microfluidic chip, roughly the size of a pack of cards. Collaborators in this groundbreaking research include Duke-NUS Medical School (Duke-NUS), Institute of Molecular and Cell Biology (IMCB) at the Agency for Science, Technology and Research (A*STAR), KK Women’s & Children’s Hospital (KKH) and Singapore General Hospital (SGH).
Credit: SMART CAMP
- This is the first demonstration of T-cell culture in a microfluidic chip the size of a pack of cards, allowing the miniaturisation of CAR T-cell production for cancer treatment
- Existing CAR T-cell manufacturing processes face significant bottlenecks, including being prone to contamination and subject to human error
- This novel method is a breakthrough in efficiency, enabling the quicker and easier production of CAR T-cells with fewer resources and a smaller footprint than existing automated manufacturing platforms.
- The method could also lead to more affordable methods of cell therapy manufacturing and even enable point-of-care manufacturing of CAR T-cells in hospitals and wards
Singapore, 27 June 2024 – Researchers from the Critical Analytics for Manufacturing Personalized-Medicine (CAMP) Interdisciplinary Research Group (IRG) at Singapore-MIT Alliance for Research and Technology (SMART), MIT’s research enterprise in Singapore, have developed a novel method capable of producing clinical doses of viable autologous chimeric antigen receptor (CAR) T-cells in a ultra-small automated closed-system microfluidic chip, roughly the size of a pack of cards. Collaborators in this groundbreaking research include Duke-NUS Medical School (Duke-NUS), Institute of Molecular and Cell Biology (IMCB) at the Agency for Science, Technology and Research (A*STAR), KK Women’s & Children’s Hospital (KKH) and Singapore General Hospital (SGH).
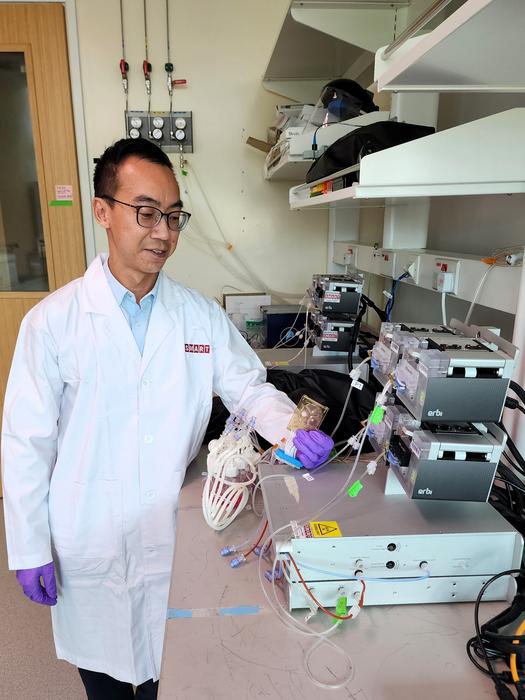
This method is the first time that a microbioreactor is used in the production of autologous cell therapy products. Specifically, the novel method was successfully used to manufacture and expand CAR-T cells that are as effective as cells produced using existing systems in a smaller footprint and less space, and using fewer seeding cell numbers and cell manufacturing reagents. This could lead to more efficient and affordable methods of scaling-out autologous cell therapy manufacturing, and could even potentially enable point-of-care manufacturing of CAR T-cells outside of a laboratory setting – such as in hospitals and wards.
CAR T-cell therapy manufacturing requires the isolation, activation, genetic modification and expansion of a patient’s own T-cells to kill tumour cells upon reinfusion into the patient. Despite how cell therapies have revolutionised cancer immunotherapy, with some of the first patients who received autologous cell therapies in remission for more than ten years, the manufacturing process for CAR-T cells has remained inconsistent, costly and time-consuming. It can be prone to contamination, subject to human error, and requires seeding cell numbers that are impractical for smaller-scale CAR T-cell production. These challenges create bottlenecks that restrict both the availability and affordability of these therapies despite their effectiveness.
In a paper titled “High-density microbioreactor process designed for automated point-of-care manufacturing of CAR T cells” published in the scientific journal Nature Biomedical Engineering, CAMP researchers detailed their breakthrough – human primary T-cells can be activated, transduced and expanded to high densities in a two-mililitre automated closed-system microfluidic chip to produce over 60 million CAR T-cells from donors with lymphoma, and over 200 million CAR T-cells from healthy donors. The CAR T-cells produced using the microbioreactor are as effective as those produced using conventional methods, but in a smaller footprint and less space, and with fewer resources. This translates to lower cost of goods manufactured (COGM) and potentially translates to lower costs for patients.
With high T-cell expansion rates, similar total T-cell numbers could be attained with a shorter culture period in the microbioreactor (7 to 8 days) compared to gas-permeable culture plates (12 days), potentially shortening production times by 30 to 40%. The researchers demonstrated that the CAR T-cells from both the microfluidic bioreactor and gas-permeable culture plates only showed subtle differences in cell quality. The cells were equally functional in killing leukaemia cells when tested in mice.
“This new method suggests that a dramatic miniaturisation of current-generation autologous cell therapy production is feasible, with the potential of significantly alleviating manufacturing limitations of CAR T-cell therapy. Such a miniaturisation would lay the foundation for point-of-care manufacturing of CAR T-cells and decrease the “good manufacturing practice” (GMP) footprint required for producing cell therapies – which is one of the primary drivers of COGM,” said Wei-Xiang Sin, Research Scientist at SMART CAMP and first author of the paper.
Notably, the microbioreactor used in the research is a perfusion-based, automated, closed system with the smallest footprint per dose, smallest culture volume and seeding cell number, as well as the highest cell density and level of process control attainable. These microbioreactors – previously only used for microbial and mammalian cell cultures – were originally developed at MIT and have been advanced to commercial production by Millipore Sigma.
The small starting cell numbers required, compared to existing larger automated manufacturing platforms, means that smaller amounts of isolation beads, activation reagents, and lentiviral vectors are required per production run. In addition, smaller volumes of medium are required (at least tenfold lower than larger automated culture systems) owing to the extremely small culture volume (2 millilitres; approximately 100-fold lower than larger automated culture systems) – which contributes to significant reductions in reagent cost. This could benefit patients, especially paediatric patients who have low or insufficient T-cell numbers to produce therapeutic doses of CAR T-cells.
“This advancement in cell therapy manufacturing could ultimately offer a point-of-care platform that could substantially increase the number of CAR T-cell production slots, reducing the wait times and cost of goods of these living medicines – making cell therapy more accessible to the masses. The use of scaled-down bioreactors could also aid process optimisation studies, including for different cell therapy products,” said Michael Birnbaum, Co-Lead Principal Investigator at SMART CAMP, Associate Professor of Biological Engineering at MIT, and a co-corresponding author of the paper.
Moving forward, SMART CAMP is working on further engineering sampling and/or analytical systems around the microbioreactor so that CAR-T production can be performed with reduced manpower and out of a laboratory setting, potentially facilitating the decentralised bedside manufacturing of CAR T-cells. SMART CAMP is also looking to further optimise the process parameters and culture conditions to improve cell yield and quality for future clinical use.
The research is conducted by SMART and supported by the National Research Foundation (NRF) Singapore under its Campus for Research Excellence and Technological Enterprise (CREATE) programme.
###
DOI
10.1038/s41551-024-01219-1
Method of Research
Experimental study
Subject of Research
Cells
Article Title
A high-density microfluidic bioreactor for the automated manufacturing of CAR T cells
Article Publication Date
4-Jun-2024