Researchers at the University of Toronto have found a way to better control the preclinical generation of key neurons depleted in Parkinson’s disease, pointing toward a new approach for a disease with no cure and few effective treatments.
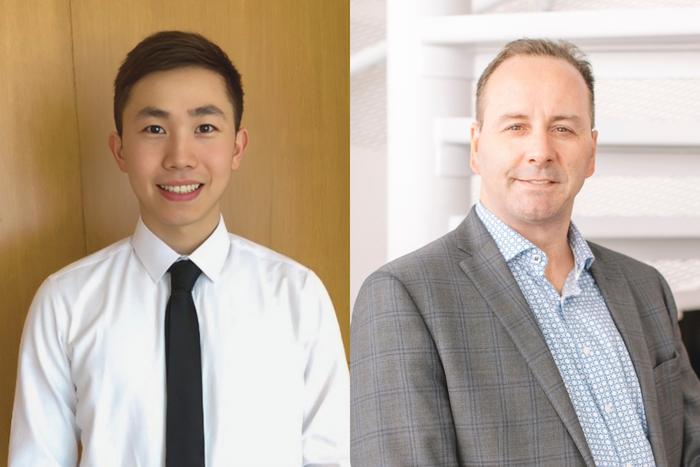
Credit: University of Toronto, Donnelly Centre for Cellular and Biomolecular Research
Researchers at the University of Toronto have found a way to better control the preclinical generation of key neurons depleted in Parkinson’s disease, pointing toward a new approach for a disease with no cure and few effective treatments.
The researchers used an antibody to selectively activate a receptor in a molecular signaling pathway to develop dopaminergic neurons. These neurons produce dopamine, a neurotransmitter critical to brain health.
Researchers around the world have been working to coax stem cells to differentiate into dopaminergic neurons, to replace those lost in patients living with Parkinson’s disease. But efforts have been hindered in part by an inability to target specific receptors and areas of the brain.
“We used synthetic antibodies that we had previously developed to target the Wnt signaling pathway,” said Stephane Angers, principal investigator on the study and director of the Donnelly Centre for Cellular and Molecular Biology.
“We can selectively activate this pathway to direct stem cells in the midbrain to develop into neurons by targeting specific receptors in the pathway,” said Angers, who is also a professor in the Leslie Dan Faculty of Pharmacy and the Temerty Faculty of Medicine, and holds the Charles H. Best Chair of Medical Research at U of T. “This activation method has not been explored before.”
The study was recently published in the journal Development.
Parkinson’s disease is the second-most common neurological disorder after Alzheimer’s, affecting over 100,000 Canadians. It particularly impacts older men, progressively impairing movement and causing pain as well as sleep and mental health issues.
Most previous research efforts to activate the Wnt signaling pathway have relied on a GSK3 enzyme inhibitor. This method involves multiple signaling pathways for stem cell proliferation and differentiation, which can lead to unintended effects on the newly produced neurons and activation of off-target cells.
“We developed an efficient method for stimulating stem cell differentiation to produce neural cells in the midbrain,” said Andy Yang, first author on the study and a PhD student at the Donnelly Centre. “Moreover, cells activated via the FZD5 receptor closely resemble dopaminergic neurons of natural origin.”
Another promising finding of the study was that implanting the artificially-produced neurons in a rodent model with Parkinson’s disease led to improvement of the rodent’s locomotive impairment.
“Our next step would be to continue using rodent or other suitable models to compare the outcomes of activating the FZD5 receptor and inhibiting GSK3,” said Yang. “These experiments will confirm which method is more effective in improving symptoms of Parkinson’s disease ahead of clinical trials.”
This research was supported by the University of Toronto Medicine by Design program, which receives funding from the Canada First Research Excellence Fund, and the Canadian Institutes of Health Research.
Journal
Development
DOI
10.1242/dev.202545
Article Title
Exploiting spatiotemporal regulation of FZD5 during neural patterning for efficient ventral midbrain specification
Article Publication Date
4-Mar-2024




