Anti-N-methyl-d-aspartate (Anti-NMDA) receptor encephalitis is an acute
autoimmune disorder that develops both neurological symptoms and psychiatric
symptoms, including hallucination, cognitive disturbance, epilepsy, movement
disorder, and impaired consciousness. This disease may be misdiagnosed at the early
stage as a psychosis disease because of primary psychiatric symptoms. The
misdiagnosis may delay appropriate therapeutic intervention. Most patients with
anti-NMDA receptor encephalitis respond to immunotherapy [1, 2].
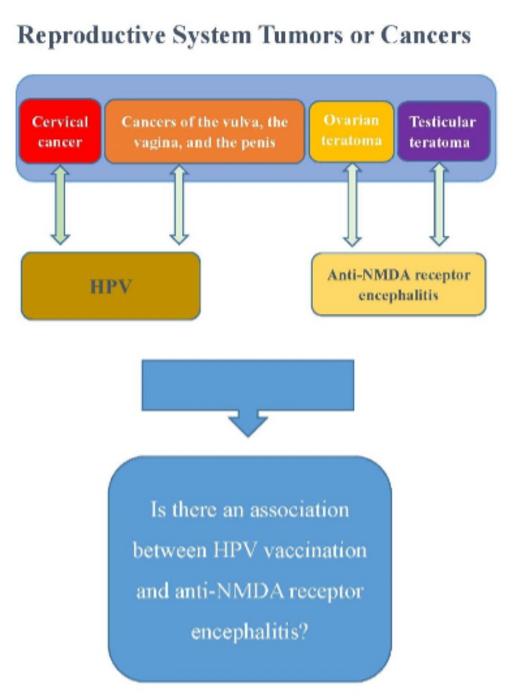
The pathology of this disease is an autoimmunity reaction that anti-NMDA
antibodies attack patients’ brains. Tumors might induce anti-NMDA receptor
immune responses due to cross-reactivity with NMDA receptors in teratomas
containing brain cells. Ovarian teratomas could trigger anti-NMDA receptor
encephalitis, and other tumors including neuroendocrine tumors, mediastinal
teratomas, testicular teratomas, and small-cell lung carcinoma have been reported
to be associated with anti-NMDA antibodies [3]. Recently, it was reported that stress
might cause this disease, and stress management may prevent relapse.
In addition to tumors and stress, other types of encephalitis or vaccinations may
trigger anti-NMDA receptor encephalitis [4-7]. Japanese encephalitis (JE) and herpes
simplex virus (HSV) encephalitis might induce anti-NMDA receptor encephalitis.
Several anti-NMDA receptor encephalitis cases have been reported to be associated
with vaccination, including JE, influenza A virus subtype H1N1,
odiphtheria/pertussis/tetanus/poliomyelitis vaccination or coronavirus disease 2019
(COVID-19) vaccinations.
In addition to these vaccines, cases of papillomavirus (HPV) vaccination triggering
anti-NMDA receptor encephalitis have been reported, but the underlying mechanism
has not been explored. HPV vaccination prevents infections with HPV, which can
cause cervical cancer (CC). CC is one of the most common cancers threatening
women's health that develops in a woman's cervix. Cases of adverse events related
Credit: Image Rights belong to Bentham Science
Anti-N-methyl-d-aspartate (Anti-NMDA) receptor encephalitis is an acute
autoimmune disorder that develops both neurological symptoms and psychiatric
symptoms, including hallucination, cognitive disturbance, epilepsy, movement
disorder, and impaired consciousness. This disease may be misdiagnosed at the early
stage as a psychosis disease because of primary psychiatric symptoms. The
misdiagnosis may delay appropriate therapeutic intervention. Most patients with
anti-NMDA receptor encephalitis respond to immunotherapy [1, 2].
The pathology of this disease is an autoimmunity reaction that anti-NMDA
antibodies attack patients’ brains. Tumors might induce anti-NMDA receptor
immune responses due to cross-reactivity with NMDA receptors in teratomas
containing brain cells. Ovarian teratomas could trigger anti-NMDA receptor
encephalitis, and other tumors including neuroendocrine tumors, mediastinal
teratomas, testicular teratomas, and small-cell lung carcinoma have been reported
to be associated with anti-NMDA antibodies [3]. Recently, it was reported that stress
might cause this disease, and stress management may prevent relapse.
In addition to tumors and stress, other types of encephalitis or vaccinations may
trigger anti-NMDA receptor encephalitis [4-7]. Japanese encephalitis (JE) and herpes
simplex virus (HSV) encephalitis might induce anti-NMDA receptor encephalitis.
Several anti-NMDA receptor encephalitis cases have been reported to be associated
with vaccination, including JE, influenza A virus subtype H1N1,
odiphtheria/pertussis/tetanus/poliomyelitis vaccination or coronavirus disease 2019
(COVID-19) vaccinations.
In addition to these vaccines, cases of papillomavirus (HPV) vaccination triggering
anti-NMDA receptor encephalitis have been reported, but the underlying mechanism
has not been explored. HPV vaccination prevents infections with HPV, which can
cause cervical cancer (CC). CC is one of the most common cancers threatening
women's health that develops in a woman's cervix. Cases of adverse events related
to HPV vaccination including chronic fatigue syndrome, postural orthostatic
tachycardia syndrome (POTS), orthostatic intolerance, and complex regional pain
syndrome have been reported. Compared to these adverse events, only a few
studies reported anti-NMDA receptor encephalitis cases that were associated with
HPV vaccination. Since cases of HPV vaccination triggering anti-NMDA receptor
encephalitis have been reported, this study investigates the underlying mechanism
from a molecular perspective. The method is based on the phylogenetic analyses of
microRNA (miRNA) biomarkers. miRNA biomarkers have been used to explore the
relationship between anti-NMDA receptor encephalitis and vaccination (or tumors).
In addition, it is worth mentioning that HPV can cause cancers, and anti-NMDA
receptor encephalitis is associated with tumors. Ovarian teratomas were the most
commonly reported anti-NMDA receptor encephalitis-associated tumor in females.
Testicular teratomas were reported to be associated with anti-NMDA receptor
encephalitis in males. HPV might induce CC and cancers of the vulva, the vagina, the
penis, and the anus. Both HPV and anti-NMDA receptor encephalitis have been
associated with tumors or cancers of the male and female reproductive systems. This
may shed light on investigating the mechanism of the association between HPV
vaccination and anti-NMDA receptor encephalitis.
While the risk of HPV triggering encephalitis appears low, the study emphasizes the
need for vigilance. Those who develop psychiatric or neurological symptoms
following HPV vaccination should undergo an evaluation for anti-NMDA receptor
encephalitis, with a thorough examination to rule out other potential complications.
References
1. Wang, H.* (2016). Efficacies of treatments for anti-NMDA receptor encephalitis,
Frontiers in Bioscience-Landmark, 21:651-63.
2. Wang, H.* (2020). Anti-NMDA Receptor Encephalitis: Efficacy of Treatment for
Male Patients and miRNA Biomarker, Current Medicinal Chemistry, 27(24):4138-
4151.
3. Wang, H.* (2019). Phylogenetic Analysis to Explore the Association Between Anti-
NMDA Receptor Encephalitis and Tumors Based on microRNA Biomarkers,
Biomolecules, 9(10), 572.
4. Wang, H.* (2017). Anti-NMDA Receptor Encephalitis and Vaccination,
International Journal of Molecular Sciences, 18, 193.
5. Wang, H.* (2018). A protocol for investigating the association of vaccination and
anti-NMDA receptor encephalitis. Frontiers in Bioscience (Scholar Edition), 10:229-
237. 6. Wang, H.* (2019). Anti-NMDA Receptor Encephalitis, Vaccination and
Viruses. Current Pharmaceutical Design, 25(43),4579-88.
7. Wang, H.* (2022). COVID-19, Anti-NMDA Receptor Encephalitis and MicroRNA.
Fronters in Immunology, 13:825103.
Journal
Current Medicinal Chemistry
DOI
10.2174/0109298673264615231124072130




