An innovative computational tool dubbed “SNAF” may help the research world bring the emerging promise of cancer immunotherapy to a wider range of patients, according to a study published Jan. 17, 2024, in Science Translational Medicine.
Credit: Cincinnati Children’s
An innovative computational tool dubbed “SNAF” may help the research world bring the emerging promise of cancer immunotherapy to a wider range of patients, according to a study published Jan. 17, 2024, in Science Translational Medicine.
The research tool, called the Splicing Neo Antigen Finder (SNAF), was developed by a multidisciplinary team of researchers from Cincinnati Children’s and the University of Virginia. The project was led by Guangyuan Li, PhD, and Nathan Salomonis, PhD, both with the Division of Biomedical Informatics at Cincinnati Children’s.
The co-authors say the tool has already helped uncover shared immunogenic targets across various cancers, which could pave the way for a new wave of highly focused cancer treatments.
“The implications of this discovery are significant,” says H. Leighton “Lee” Grimes, PhD, a co-author of the study and director of the Cancer Pathology Program at Cincinnati Children’s. “By identifying shared splicing neoantigens present in up to 90% of cancer patients, SNAF not only presents new targets for therapy but also challenges and expands our understanding of cancer biology.”
How the new tool finds new targets
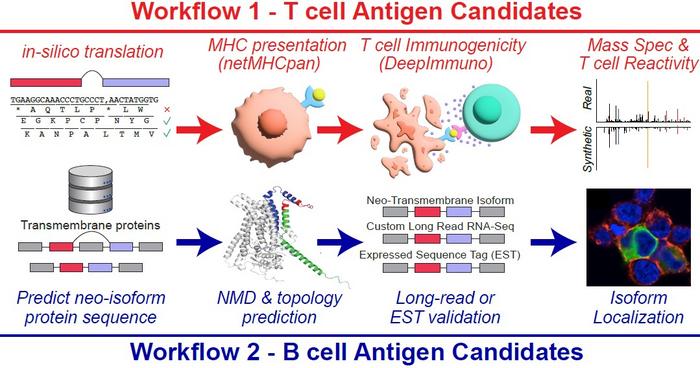
Immunotherapy, which harnesses a patient’s immune system to fight cancer, often targets neoantigens produced from genetic mutations. However, this approach typically benefits only those with a high mutational burden. SNAF aims to expand the universe of immunotherapy by identifying neoantigens arising from post-transcriptional modifications, particularly splicing errors, which have been largely untapped until now.
Using new artificial intelligence approaches, SNAF predicts immunogenic peptides that T cells can recognize and novel proteins with altered extracellular components that B cells can target. This dual approach is vital in developing comprehensive immunotherapies that engage both arms of the adaptive immune system.
Promising target emerges for melanoma
While cataloging all possible neoantigens produced from alternative mRNA pathways, the team found that the amount of splicing neoantigens is correlated with patient survival and responses to immunotherapy in patients with melanoma.
One such prediction, SLC45A2, has emerged as a particularly promising target due to its high tumor specificity and immunogenicity.
In addition to T-cell neoantigens, the team has discovered a novel class of tumor-specific extracellular neo-epitopes, termed ExNeoEpitopes, through their B-cell focused pipeline, SNAF-B. These ExNeoEpitopes show great promise for the development of monoclonal antibodies and CAR-T cell therapies.
Next steps
“This is only the beginning,” says Tamara Tilburgs, PhD, co-corresponding author and a researcher in the Division of Immunobiology. “The SNAF workflow’s flexibility means it can be continuously adapted as we make further inroads into understanding and combating cancer.”
Salomonis and his team are now applying these tools in the most difficult-to-treat cancers to find the best targets for therapy development and understand their single-cell origins.
The research was supported by multiple grants, including the Cincinnati Children’s Hospital Research Foundation, the University of Cincinnati Cancer Center, the Melanoma Research Foundation, the American Cancer Society, and the National Institutes of Health (R01CA226802).
Journal
Science Translational Medicine
DOI
10.1126/scitranslmed.ade2886
Method of Research
Computational simulation/modeling
Article Title
Splicing neoantigen discovery with SNAF reveals shared targets for cancer immunotherapy
Article Publication Date
17-Jan-2024
COI Statement
The co-authors report no conflicts.




