Washington D.C.—The December Health Affairs, a theme issue about the lessons learned around the globe from the COVID-19 pandemic, covers topics including how modeling was used to respond to the pandemic, how health inequities emerged and were addressed, and how countries tried to protect their vulnerable residents. The December issue of Health Affairs was supported by the Robert Wood Johnson Foundation and the Merck Foundation.
Credit: Health Affairs
Washington D.C.—The December Health Affairs, a theme issue about the lessons learned around the globe from the COVID-19 pandemic, covers topics including how modeling was used to respond to the pandemic, how health inequities emerged and were addressed, and how countries tried to protect their vulnerable residents. The December issue of Health Affairs was supported by the Robert Wood Johnson Foundation and the Merck Foundation.
There will be a Health Affairs briefing on Tuesday, December 5, from 11:00 a.m. to 2:00 p.m. ET. Register here.
COVID-19, a decline in FDA foreign facility inspections.
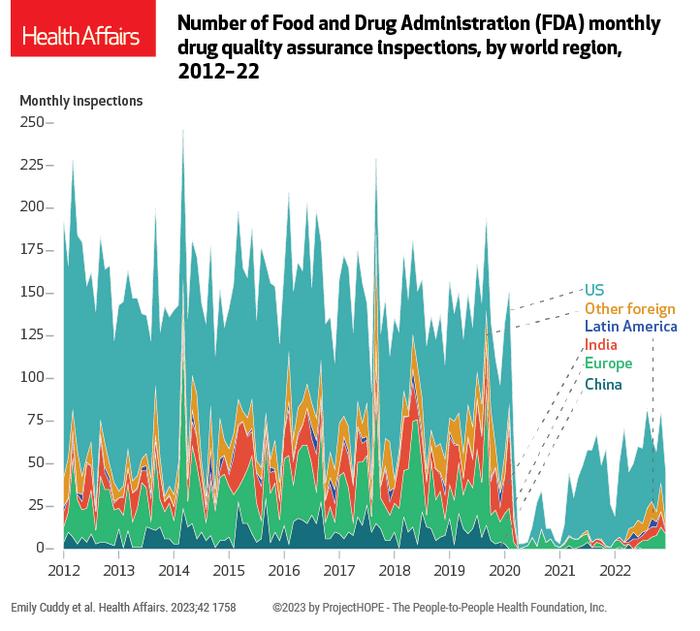
At the start of the COVID-19 pandemic, the Food and Drug Administration (FDA) halted inspections of most overseas drug and manufacturing establishments. To understand the consequences of this policy change for both domestic and foreign inspections, Emily Cuddy of Duke University and coauthors looked at data on inspections performed by the FDA Office of Regulatory Affairs for the period 2012–22. They found that by 2022, compared with 2019 rates, total annual domestic inspections had decreased approximately 35 percent and total foreign inspections had declined about 79 percent. (See exhibit below.) According to the authors, the decrease in inspection activity did not correspond to a decrease in drug manufacturing activity, and the FDA investigator workforce during the pandemic was also stable. They noted that the COVID-19 pandemic increased the costs and complexity of conducting inspections, especially those abroad. Furthermore, about 70 percent of inspections during the pandemic were reinspections of establishments with a history of objectionable conditions; more randomly selected surveillance inspections were essentially paused. The authors conclude that their findings could indicate growing quality issues in the industry and raise questions about the feasibility of clearing the inspection backlog with currently available resources.
[ADD IMAGE]
The effects of care disruptions in Latin America.
COVID-19 hit Latin America harder than any other region of the world: According to data from the Inter-American Development Bank, the area accounted for about 30 percent of global deaths from COVID-19, even though it only has 8 percent of the world’s population. Disruptions in health care services were experienced around the world, but to date there has been little research on the implications of their effect on public health. To provide regional evidence, and to describe changes in hospitalization and excess mortality for non-COVID-19-related illness in Latin America during the pandemic, Pedro Bernal Lara of the Inter-American Development Bank and coauthors studied changes in hospitalizations and mortality during the pandemic, focusing on conditions for which access to timely and effective health care can prevent premature death. They examined government data for March 2020–December 2021 from four countries (Brazil, Ecuador, Mexico, and Peru) and found that hospitalization rates for these conditions declined by 28 percent and mortality increased by 15 percent relative to prepandemic years, with the poorest states in each country experiencing larger increases in mortality. According to the authors, disruptions in hospital care for noncommunicable diseases, such as cardiovascular diseases, diabetes, and renal failure, had the most severe health consequences. The authors recommend that policy makers focus on building resilient essential health services that can be maintained during emergencies by ensuring coordinated and continuous care through means such as telemedicine, broadening the role of nonphysical health care workers, and expanding options for medication delivery.
Reasons for vaccine uptake inequities in the Western Pacific and parts of Africa.
Low- and middle-income countries around the world have struggled with vaccine access, distribution, and uptake during the COVID-19 pandemic. The gap in vaccine availability between high- and low-income countries has been described as “vaccine apartheid,” yet much of the existing research has focused on reducing vaccine hesitancy to increase demand for vaccines. To better understand how vaccine availability and demand in these regions affect uptake, Ashley Fox of the University of Albany, State University of New York, and coauthors from the London School of Hygiene and Tropical Medicine reviewed survey data collected from 15,696 respondents in seventeen low- and middle-income countries in the Western Pacific and Africa regions between May 2022 and January 2023. The authors found that 14 percent of the sample reported unmet immunization demand; in sub-Saharan African countries alone, reported unmet demand ranged from 11 percent to 43 percent. According to the authors, among the 4,388 respondents in the two regions who had not been vaccinated for COVID-19, 50 percent were still willing to get vaccinated, particularly in African countries. For those not willing to be vaccinated, the most frequent reason given was a diminished perception of the COVID-19 risk, which the authors found to be a shift from earlier in the pandemic, when concerns about the safety of the vaccination appeared to be the dominant reason. The authors recommend renewed policy efforts to address barriers to vaccine access in countries with low coverage, as well as messaging to overcome vaccine hesitancy, to achieve higher vaccination rates across regions.
Also of interest in the December issue:
- Global Vaccine Access Demands Combating Both Inequity And Hesitancy; Peter Hotez of Baylor College of Medicine
- Live Versus Livelihoods: The Epidemiological, Social, And Economic Impact Of COVID-19 In Latin American And The Caribbean; Adolfo Rubinstein of the Institute for Clinical Effectiveness and Health Policy and coauthors
- Adolescent Social Outcomes Declined During COVID-19: Evidence From Bangladesh, Jordan, And Ethiopia; Jennifer Seager of The George Washington University and coauthors
- Published Ahead Of Print on November 15: A Systematic Review Of COVID-19 Misinformation Interventions: Lessons Learned; Rory Smith and coauthors from Brown University
# # #
Health Affairs is the leading peer-reviewed journal at the intersection of health, health care, and policy. Published monthly by Project HOPE, the journal is available in print and online. Late-breaking content is also found through healthaffairs.org, Health Affairs Today, and Health Affairs Sunday Update.
Health Affairs podcasts go beyond the journal’s pages to bring you insightful discussions on the latest news and research affecting health policy. On our flagship podcast, A Health Podyssey, Editor-In-Chief Alan Weil interviews the leading researchers and influencers shaping the field’s big ideas. Join Health Affairs editors on Health Affairs This Week as they discuss the week’s most pressing health policy news. All in 15 minutes or less.
Project HOPE is a global health and humanitarian relief organization that places power in the hands of local health care workers to save lives across the globe. Project HOPE has published Health Affairs since 1981.
Journal
Health Affairs




