Hepatitis B virus (HBV) is a significant public health problem, with over 296 million people chronically infected worldwide. Despite the availability of a safe and effective vaccine for over 40 years, HBV remains a leading cause of liver disease and death.
Credit: By Armando Andres Roca Suarez and Fabien Zoulim
Hepatitis B virus (HBV) is a significant public health problem, with over 296 million people chronically infected worldwide. Despite the availability of a safe and effective vaccine for over 40 years, HBV remains a leading cause of liver disease and death.
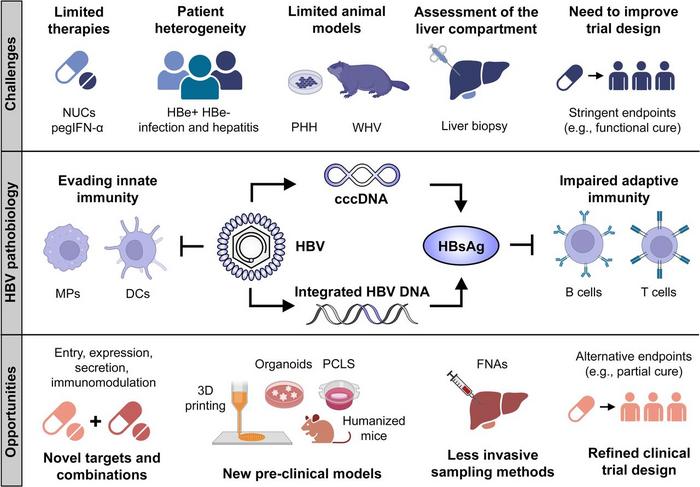
One of the main challenges to curing HBV is the unique biology of the virus. HBV replicates through a covalently closed circular DNA (cccDNA) intermediate integrated into the host genome. This makes it very difficult to eradicate the virus completely, even with effective antiviral therapy. Another challenge is the impaired immune response to HBV in chronically infected individuals. The virus has evolved several mechanisms to evade the immune system, making it difficult for the body to clear the infection.
The currently available antivirals, i.e. nucleos(t)ide analogues, are not curative, and long-term therapy is required to suppress viral replication and prevent complications such as cirrhosis and hepatocellular carcinoma (HCC). In recent years, there has been significant progress in developing new antiviral drugs and immunotherapies for HBV to cure the infection with a finite duration of treatment.
One promising new therapeutic approach is the use of immune-based therapies. These therapies aim to boost the host immune response to HBV and help the body clear the virus. Several immune-based therapies are currently in clinical development, including vaccines, adoptive T-cell therapy, and gene therapy.
Another promising approach is the development of curative combinations. These combinations combine different therapies, such as antiviral drugs and immune-based therapies, to achieve a cure for HBV. Some curative combinations are currently in clinical development, and there is hope that a cure for HBV may be within sight.
In addition to the biological challenges to curing HBV, there are also a number of clinical challenges. One challenge is the lack of a definitive cure endpoint. Currently, a functional cure is defined as sustained loss of HBsAg (a surface antigen of HBV) for at least 6 months after treatment. However, this does not guarantee that the virus has been completely eradicated from the body, as cccDNA may still be present. Thus, restoring HBV-specific immune responses is critical to control the residual infection. The discovery and validation of novel biomarkers predicting functional cures will be important for monitoring the new therapies and for treatment personalization.
Despite the challenges, significant progress is being made in developing new curative strategies for HBV. The new understanding of HBV biology and antiviral immune responses has led to identifying new drug targets and a renewed interest in developing curative combinations. Ongoing clinical trials are evaluating the safety and efficacy of these new approaches and will pave the way for a functional cure for HBV infection.
See the article:
Roca Suarez AA, Zoulim F. Opportunities and challenges for hepatitis B cure. eGastroenterology 2023;1:e100021. doi:10.1136/egastro-2023-100021
About the eGastroenterology
eGastroenterology is a new, open-access, and open peer-reviewed BMJ Journal, which focuses on basic, clinical, translational, and evidence-based medicine research in all areas of gastroenterology (including hepatology, pancreatology, esophagology, and gastrointestinal surgery).
For more information, please visit: egastroenterology.bmj.com and follow us on Twitter (@eGastro_BMJ).
Sign-up to Email Alerts for eGastroenterology: https://emails.bmj.com/k/Bmj/jausu/egastroenterology
Journal
eGastroenterology
DOI
10.1136/egastro-2023-100021
Article Title
Opportunities and challenges for hepatitis B cure




