The Eunice Kennedy Shriver National Institute of Child Health and Human Development awarded $3.1 million to the University of Arkansas to study a spectrum of pediatric mitochondrial disorders caused by mutations in the mitochondria. These disorders often impact different organs requiring energy and can lead to mitochondria-induced multiple organ disorder syndromes, or MIMODS.
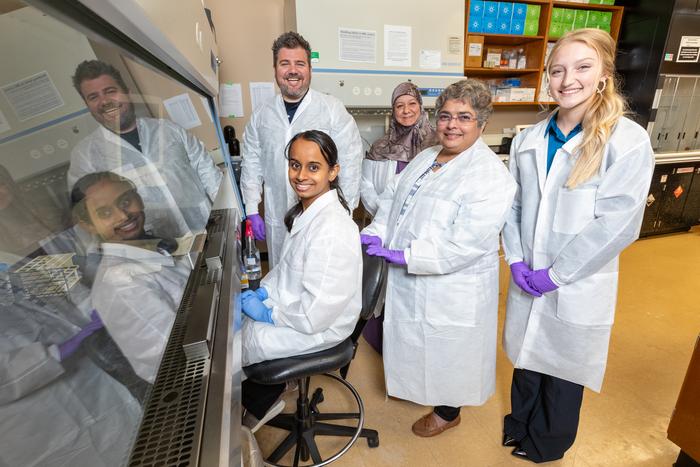
Credit: University Relations
The Eunice Kennedy Shriver National Institute of Child Health and Human Development awarded $3.1 million to the University of Arkansas to study a spectrum of pediatric mitochondrial disorders caused by mutations in the mitochondria. These disorders often impact different organs requiring energy and can lead to mitochondria-induced multiple organ disorder syndromes, or MIMODS.
Shilpa Iyer, an associate professor of biological sciences, will serve as the principal investigator on the five-year award. Iyer and her team conduct research on mitochondrial diseases and have received grants from Arkansas Bioscience Institute, National Institute of Health and the Department of Defense. Her team has obtained skin cells from mitochondrial patients and are creating disease-specific stem cells to better understand the role of bioenergetics and mitochondrial mutations in vital tissue types — such as the heart, nerve, muscle, and kidney — that are affected by mitochondrial diseases.
Mitochondria, the tiny organelles inside cells, play a critical role in producing metabolic energy by oxidizing carbohydrates, protein and fats. In the presence of oxygen, this organelle combines with glucose and fats to create ATP, or adenosine triphosphate, which is the energy fuel for sustaining life. Many devastating diseases can arise from damage to mitochondria and could contribute to MIMODS in children and adults alike.
The NIH award will be used to explore how damage to the mitochondria alters the shape of the mitochondria and adversely impacts bioenergetic function, which in turn can affect the proper functioning of the organs, leading to disease severity and organ failure. The award will test the hypothesis that the causative role of specific metabolites altered by mutations in the mitochondrial genome lead to organ failure in pediatric mitochondrial disorders.
“Starting with skin cells from children with mitochondrial disorders, our team is involved in recreating cells in vital organs impacted by the disease to capture many aspects of disease progression, which could lead to better understanding of mitochondria mutations and multiple organ failure,” Iyer said. “It is our hope that results from these studies will provide new therapies for patients impacted by mitochondrial disorders.”
Iyer reasons that the team’s interdisciplinary expertise in mitochondrial genetics and physiology, stem cell biology and differentiation, next-generation sequencing analysis and metabolite profiling supported by animal studies, will provide new directions for exploring the complexities associated with mitochondrial disorders.
In addition to Raj Rao, a professor of biomedical engineering, and Chris Nelson, an assistant professor of biomedical engineering, both with the U of A, Iyer’s team includes Franklin West, at the Regenerative Bioscience Center at the University of Georgia; Sean Palecek, at the Department of Chemical and Biological Engineering at the University of Wisconsin, Madison; Edward J. Lesnefsky Jr., at the Richmond VA Medical Center; and Thomas LaFramboise, at the Department of Genetics and Genome Sciences, Case Western Reserve University.
The North American Mitochondrial Disease Consortium, the Children’s Hospital of Salzburg and Innsbruck, and the Jackson Laboratory are also providing additional support and resources.
The announcement of this award also coincides with World Mitochondrial Disease Awareness Week Sept. 18-24.




