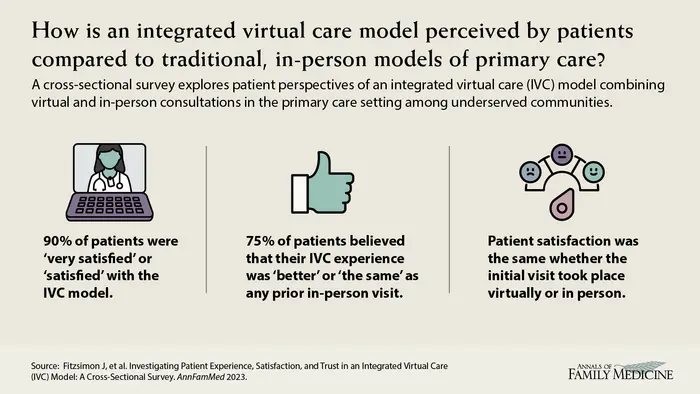
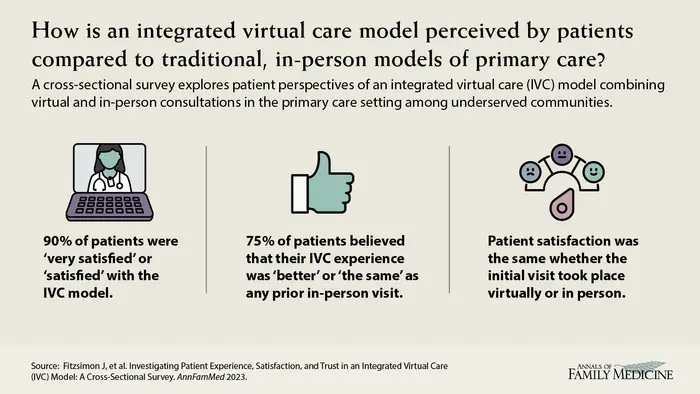
In an effort to increase access to care in underserved communities, researchers from the University of Ottawa evaluated the implementation of an integrated virtual care (IVC) model. Their study evaluated the overall experience and satisfaction of patients receiving care through a combination of virtual and in-person visits. A secondary aim was to compare the experiences of patients who had been previously seen in person by a family physician before transitioning to the IVC clinics with those who met their family physician virtually for the first time in their virtual appointment at participating clinics.
Credit: Annals of Family Medicine
In an effort to increase access to care in underserved communities, researchers from the University of Ottawa evaluated the implementation of an integrated virtual care (IVC) model. Their study evaluated the overall experience and satisfaction of patients receiving care through a combination of virtual and in-person visits. A secondary aim was to compare the experiences of patients who had been previously seen in person by a family physician before transitioning to the IVC clinics with those who met their family physician virtually for the first time in their virtual appointment at participating clinics.
The IVC model helps alleviate the burden on overwhelmed primary care clinicians by leveraging telemedicine technology, allowing family doctors located outside the community to provide care to patients remotely. By utilizing secure messaging, telephone consultations, and video appointments, the IVC model expands the pool of available family doctors, ensuring patients can access care even when local clinicians are overburdened. In-person care is provided by physicians, nurse practitioners and other allied health professionals including community paramedics within the local family health team.
Using a cross-sectional online survey administered to 121 patients, the researchers determined that across all groups, 90% of patients were very satisfied or satisfied with care from their family physician, and 89% with care from their allied health team. When comparing previous healthcare experiences, 75% of respondents believe that their encounters with IVC were better than or the same as any prior, in-person healthcare encounters. There was no difference in satisfaction or trust between patients who had a previously established in-person relationship with their doctor and those whose first visit was virtual.
What We Know: Health care systems, both in Canada and globally, have long faced challenges in delivering timely and continuous primary care to their populations. The COVID-19 pandemic further exacerbated these difficulties, prompting health care organizations to establish virtual care networks to address the evolving needs of patients and ensure access to health care services.
What This Study Adds: Researchers found across all groups, 90% of patients were very satisfied or satisfied with care from their family physician, and 89% with care from their allied health team. When comparing previous healthcare experiences, 75% of respondents believe that their encounters with IVC were better than or the same as any prior, in-person healthcare encounters. Those levels were comparable to traditional in-person models of primary care.
Investigating Patient Experience, Satisfaction, and Trust in an Integrated Virtual Care (IVC) Model: A Cross-Sectional Survey
Jonathan Fitzsimon, MD, et al
Faculty of Medicine and Department of Family Medicine, University of Ottawa, Ontario, Canada
Permanent link
Journal
The Annals of Family Medicine