The study of biomarkers in the brain—powered by cutting-edge machine learning techniques—could redefine the way mental health conditions are categorized and diagnosed and lead to more effective, personalized treatments.
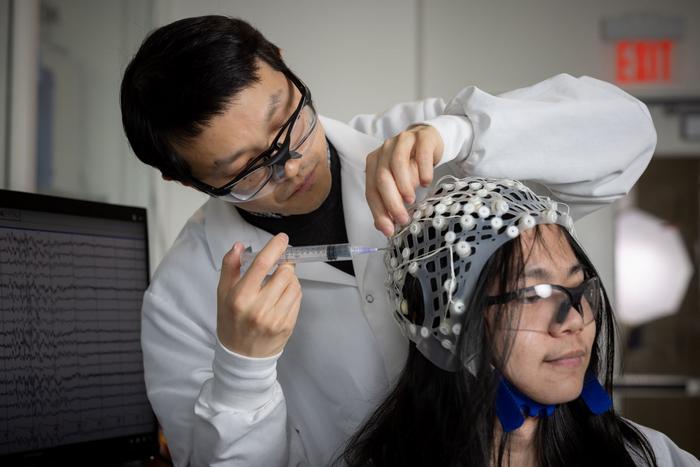
Credit: Douglas Benedict/Academic Image for Lehigh University
The study of biomarkers in the brain—powered by cutting-edge machine learning techniques—could redefine the way mental health conditions are categorized and diagnosed and lead to more effective, personalized treatments.
That’s the goal of Yu Zhang, an assistant professor of bioengineering and electrical and computer engineering in Lehigh University’s P.C. Rossin College of Engineering and Applied Science who recently landed major support from the National Institute of Mental Health (NIMH), a division of the National Institutes of Health (NIH). The two grants, which total nearly $4 million, will fund two projects searching for biomarkers using brain imaging and machine learning (ML) to improve diagnosis and treatment outcomes for patients with mental health disorders.
A biomarker is essentially a sign of some type that indicates a medical state and can be measured.
The first study aims to improve the treatment of depression. Approximately 280 million people around the world have the condition, according to the World Health Organization. Antidepressants are the primary form of treatment, but they are effective in only about half of patients who take them, says Zhang, who leads the Brain Imaging and Computation Laboratory (BIC Lab) at Lehigh.
“Traditionally, medical professionals use a combination of behavioral and clinical symptoms to diagnose depression, and those symptoms are fairly subjective and cause substantial heterogeneity in the patients,” he says. “Our goal is to build objective biomarkers using brain imaging and machine learning that better capture the brain’s dysfunction. Those biomarkers will essentially enable us to predict whether an individual patient will respond to medication based on their brain circuits, and that will help guide personalized intervention.”
Zhang and his team, which includes collaborators from Dell Medical School (Dell Med) at the University of Texas at Austin, the Perelman School of Medicine (PSOM) at the University of Pennsylvania, and Stanford University School of Medicine, will utilize data from a double-blind randomized placebo-controlled clinical trial for the biomarker establishment. Those data, including functional magnetic resonance imaging (fMRI) and electroencephalography (EEG) collected from patients prior to treatment, will be used to train a machine-learning model to identify biomarkers in the brain.
“Instead of single brain regions, the biomarker we are looking for is characterized by the interaction between different regions and between brain imaging modalities,” says Zhang. “We’re looking at large-scale brain networks related to a variety of psychiatric disorders, mainly involving cognitive working memory and emotional regulation. We hypothesize that the interaction between these intrinsic brain networks might reveal informative biomarkers that can predict individual-level treatment response.”
Essentially, he says, the degree of interaction between the networks may indicate the degree by which a person would respond to medication.
Once the team builds the model, they’ll test it by conducting an independent clinical trial. Investigators at Dell Med will recruit approximately 50 people diagnosed with depression, prescribe them antidepressant medication, and measure the change in their symptoms.
“And we’ll be collecting pretreatment brain imaging data and using that data to verify and optimize our biomarker findings,” says Zhang.
He envisions a future where the model—which would be easily installed on any computer—works in tandem with a portable EEG device.
A clinic or hospital patient would have their brain scanned by the EEG, and that data would be fed into the model. The model would use those brain signals to assess the strength or weakness of the connections between regions of the brain—i.e., the biomarkers—and then generate output that tells the doctor or clinician how well, or not, the person would likely respond to antidepressant medication based on those biomarkers.
While Zhang and his team are looking only at selective serotonin reuptake inhibitors, or SSRIs, the ultimate goal, he says, is to fine-tune the model enough that it can predict a person’s response to other compounds.
Their AI-guided biomarker would not only deliver a personalized approach to treatment, he says, but also replace the current trial-and-error treatment strategy that wastes both time and money.
“Often, for patients, time is even more important than money,” says Zhang. “So combining cutting-edge artificial intelligence with brain imaging could really drive a novel treatment solution that helps people quickly, and gives them greater confidence about their treatment. This could be a form of precision mental-health care that could offer patients real hope.”
Zhang’s second newly funded study will also use brain imaging data to identify biomarkers, this time to redefine the classification of mental disorders.
Currently, mental health conditions are grouped according to subjective behavioral and clinical assessments and self-reported questionnaires, says Zhang. The result is that within a single diagnostic category such as autism, the range of symptoms can be vast.
“Some patients show very different—or heterogenous—symptoms compared with other patients within that autism category,” he says. “At the same time, across categories like autism, attention-deficit/hyperactivity disorder, and depression, you’ll find there’s considerable overlap, or comorbidity, in symptoms. We believe there is a lack of in-depth understanding of the heterogeneity and comorbidity in major psychiatric disorders. Our project will collect more objective measures from the human body. We’ll combine brain imaging data with machine learning to identify neurocircuit abnormalities across traditional diagnoses that will help us redefine the classification of mental disorders.”
Redefining the classification system could facilitate the development of more effective treatment for patients, says Zhang. Right now, patients diagnosed with a specific disorder are generally treated with a one-size-fits-all approach. Some patients will respond well, but others won’t respond at all, and still others may experience adverse reactions. And that’s because of the wide variation in how their brains work. If the system could be more fine-tuned, treatments such as medication, psychotherapy, and neuromodulation therapy could be better dialed toward specific needs.
Zhang and his team will feed brain imaging and behavioral assessment data into a machine learning model that will identify brain connectivity patterns. Those biomarkers will help explain mental health conditions along more of a continuum.
“Right now, a diagnosis is like a hard label, but we think that explaining these conditions along a spectrum will help us identify subpopulations within a clinical sample,” he says. “Once we identify these subtypes, we can further study their unique and shared brain abnormalities, and better understand what treatment will be most useful for that specific subtype.”
The idea is that eventually doctors would initially collect both brain imaging and behavioral data from a patient, feed it into the model to learn in which subtype the patient belongs, and then proceed with the treatment suited to that subtype.
“This work has the potential to redefine mental health conditions, and would be a major breakthrough in the field,” says Zhang. “It could help us establish more effective therapeutics for individual patients, which is something traditional clinical diagnoses can’t achieve.”
Research reported in this story is supported by the National Institute of Mental Health of the National Institutes of Health under award numbers R01MH129694 and R21MH130956.
Related Links
- Rossin College Faculty Profile: Yu Zhang
- Lehigh University: Brain Imaging and Computation Laboratory (BIC Lab)
- NIH RePorter: Establishing Multimodal Brain Biomarkers Using Data-driven Analyticsfor Treatment Selection in Depression
- NIH RePorter: Identifying Transdiagnostic Functional Connectivity Biomarkers for Cognitive Health and Psychopathology
- Lehigh University: Institute for Data, Intelligent Systems, and Computation (I-DISC)




