Stem cells from the human stomach can be converted into cells that secrete insulin in response to rising blood sugar levels, offering a promising approach to treating diabetes, according to a preclinical study from researchers at Weill Cornell Medicine.
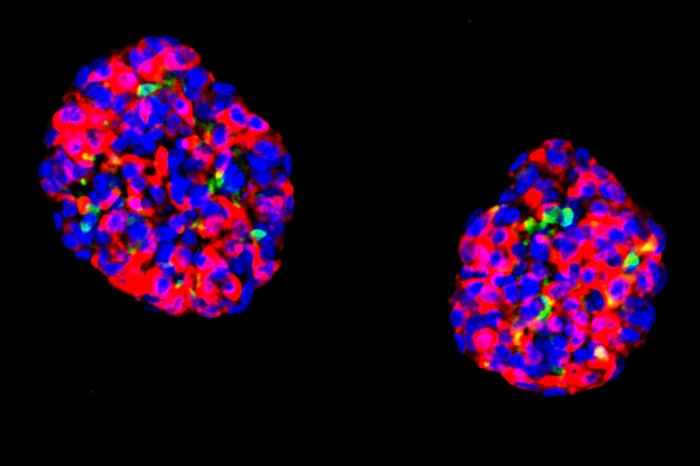
Credit: Image courtesy of Xiaofeng Huang.
Stem cells from the human stomach can be converted into cells that secrete insulin in response to rising blood sugar levels, offering a promising approach to treating diabetes, according to a preclinical study from researchers at Weill Cornell Medicine.
In the study, which appeared April 27 in Nature Cell Biology, the researchers showed that they could take stem cells obtained from human stomach tissue and reprogram them directly—with strikingly high efficiency—into cells that closely resemble pancreatic insulin-secreting cells known as beta cells. Transplants of small groups of these cells reversed disease signs in a mouse model of diabetes.
“This is a proof-of-concept study that gives us a solid foundation for developing a treatment, based on patients’ own cells, for type 1 diabetes and severe type 2 diabetes,” said study senior author Dr. Joe Zhou, a professor of regenerative medicine and a member of the Hartman Institute for Therapeutic Organ Regeneration at Weill Cornell Medicine.
Insulin is a hormone that regulates blood glucose levels—without it, blood glucose becomes too high, causing diabetes and its many complications. An estimated 1.6 million Americans have type 1 diabetes, which results from an autoimmune attack that destroys beta cells in the pancreas. At least several million other Americans lack sufficient beta cells due to severe type 2 diabetes. Current treatments in such cases include manual and wearable-pump injections of insulin, which have multiple drawbacks including pain, potentially inefficient glucose control, and the necessity of wearing cumbersome equipment.
Biomedical researchers aim to replace beta-cell function in a more natural way, with transplants of human cells that work as beta cells do: automatically sensing blood sugar levels and secreting insulin as needed. Ideally, such transplants would use patients’ own cells, to avoid the problem of transplant rejection.
Dr. Zhou has been working toward this goal for more than 15 years. In early experiments as a postdoctoral researcher, he discovered that ordinary pancreatic cells could be turned into insulin-producing beta-like cells by forcing the activation of three transcription factors—or proteins that control gene expression—resulting in the subsequent activation of genes required for the development of normal beta cells. In a 2016 study, again in mice, he and his team showed that certain stem cells in the stomach, called gastric stem cells, are also highly sensitive to this three-factor activation method.
“The stomach makes its own hormone-secreting cells, and stomach cells and pancreatic cells are adjacent in the embryonic stage of development, so in that sense it isn’t completely surprising that gastric stem cells can be so readily transformed into beta-like insulin-secreting cells,” Dr. Zhou said.
Attempts to reproduce these results using human gastric stem cells, which can be removed from patients relatively easily in an outpatient procedure called endoscopy, were slowed by various technical hurdles. However, in the new study, led by first author Dr. Xiaofeng Huang, an instructor of molecular biology in medicine at Weill Cornell Medicine, the researchers at last achieved success.
After turning human gastric stem cells into beta-like cells, the team grew the cells in small clusters called organoids and found that these organ-like pieces of tissue quickly became sensitive to glucose, responding with secretions of insulin. When transplanted into diabetic mice, the beta-like organoids functioned largely as real pancreatic beta cells would, secreting insulin in response to rises in blood glucose, and thereby keeping blood glucose levels steady. The transplants also kept working for as long as the researchers monitored them—six months—suggesting good durability.
Dr. Zhou said that he and his lab still need to optimize their method in various ways before it can be considered for clinical use. Necessary improvements include methods to increase the scale of beta-cell production for transplants to humans, and modifications of the beta-like cells to make them less vulnerable to the type of immune attack that initially wipes out beta cells in type 1 diabetes patients.
Ultimately, the researchers hope to develop a technique enabling the relatively easy harvesting of gastric stem cells from patients, followed by the transplant, weeks later, of insulin-secreting organoids that regulate blood sugar levels without the need for further medication.
Journal
Nature Cell Biology




