On World Tuberculosis (TB) Day 2023, the European Centre for Disease Prevention and Control (ECDC) and the World Health Organization (WHO) Regional Office for Europe are issuing a sobering warning that, despite having the tools to end TB, the European Region remains a long way from meeting its End TB Strategy targets of reducing TB incidence by 80% and TB deaths by 90% before 2030. Although this is partly due to the COVID-19 pandemic’s region-wide impact on health systems, including the capacity to prevent, diagnose and treat TB, countries still need to urgently renew their efforts if these targets are to be met.
Credit: ECDC
On World Tuberculosis (TB) Day 2023, the European Centre for Disease Prevention and Control (ECDC) and the World Health Organization (WHO) Regional Office for Europe are issuing a sobering warning that, despite having the tools to end TB, the European Region remains a long way from meeting its End TB Strategy targets of reducing TB incidence by 80% and TB deaths by 90% before 2030. Although this is partly due to the COVID-19 pandemic’s region-wide impact on health systems, including the capacity to prevent, diagnose and treat TB, countries still need to urgently renew their efforts if these targets are to be met.
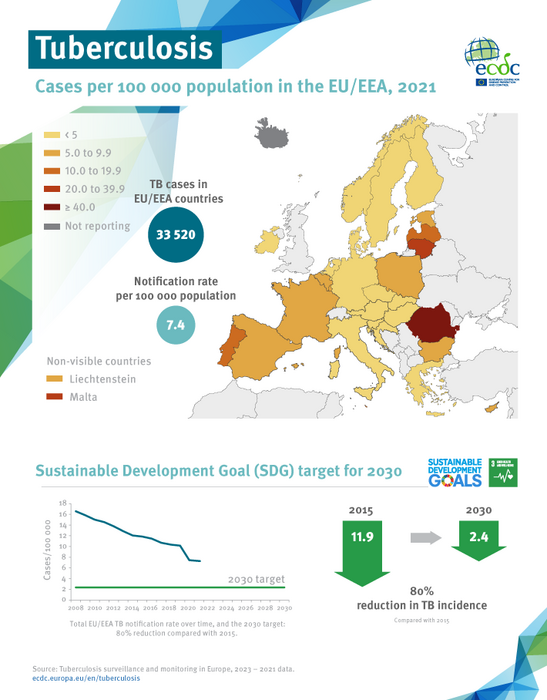
The latest ECDC/WHO report on TB surveillance and monitoring shows that, despite an overall downward trend in the incidence of TB in the WHO European Region, the current rate of decline will not be sufficient to meet targets under the United Nations Sustainable Development Goals for ending the TB epidemic by 2030.
Diagnosis and treatment are key
To end TB, it is necessary to interrupt transmission by identifying people with active TB in time and preventing the development of TB in those already infected. Despite many countries in the WHO European Region reporting a year-on-year increase in the number of notified TB cases, the Region still recorded 23% fewer TB cases in 2021 than in 2019. The Region comprises 53 countries with a population of nearly 900 million people, around 508 million of whom live in the EU/EEA (27 EU Member States plus Iceland, Liechtenstein, and Norway). Other major challenges in the Region include an increased burden of drug-resistant cases and below-target treatment success rates, combined with the disruption to TB services caused by the COVID-19 pandemic.
According to ECDC Director, Andrea Ammon, “In 2021, the raging COVID-19 pandemic continued to heavily affect our Member States. TB resources were diverted, and patients experienced difficulties in accessing clinical services, possibly resulting in delayed diagnosis and treatment of some TB cases. Therefore, we need to increase the number of people diagnosed and successfully treated. ECDC remains committed to partnering with and supporting EU/EEA countries in their efforts to end the TB epidemic.”
Just three years ago, prior to the pandemic, the Region was experiencing the fastest decline in TB incidence and mortality in the world. Yet in 2021, TB mortality in the Region increased compared to 2020, and the declining incidence curve has stalled for the first time in 20 years.
Time to act
“Despite the challenges, these are remarkable times,” said Dr Hans Henri P. Kluge, Regional Director at WHO/Europe. “We must take full advantage of new technologies, such as rapid molecular diagnoses; better and shorter regimens for prevention, treatment and care; and innovative digital health solutions.”
As Dr Kluge points out, “We have the scientific and medical tools to recoup lost ground, but we urgently need stronger, consistent, invested partnerships between Member States, donor agencies and affected communities if we are to reach everyone living with TB to give them the treatment and care they need. This September, at the second UN High-Level Meeting on TB, leaders from Europe and beyond will commit to new targets and set new milestones to end TB. These commitments will be a promise we make to help people who are most in need – as TB is largely a disease of poverty and neglect, shrouded in stigma and discrimination, affecting some of the most vulnerable. Now is the right time to chart a renewed trajectory towards ending TB in the European Region, and globally, once and for all.”
——ends—–
Note to editors
Cases reported
In 2021, there were over 166 000 new and relapse TB cases notified in the wider Region. In 2020, there were around 164 000 new and relapse TB diagnoses, and 216 000 in 2019. Many countries reported a year-on-year increase in the number of notified TB cases against 2020 and, overall, there was a slight (1.1%) recovery in TB notifications.
In 2021, 33 520 TB cases were reported in the EU/EEA. In 2020, there were over 33 800 cases reported, and 45 192 in 2019. Although country-specific notification rates differed considerably, the overall notification rate in most countries has decreased over the last five years and especially during the past two years. Although this represents a continuation of the downward trend observed since the launch of TB surveillance, recent years should be seen within the context of the COVID-19 pandemic and the challenges this created for TB clinical services and surveillance.
Drug-resistant TB
In the Region, the burden of rifampicin-resistant (RR) TB is estimated to have increased. One in three cases of pulmonary TB in the Region is resistant to rifampicin. Only 62% of pulmonary TB patients are aware of their rifampicin resistance status, and around 30% of rifampicin-resistant patients are also resistant to fluoroquinolones.
In the EU/EEA, of the 16 895 cases with drug susceptibility test results for rifampicin (as a minimum, given that the resistance of other drugs can be tested as well) reported in 2021, 630 (3.8%) involved multidrug-resistant (MDR)-TB.
Treatment success rates
Both in the EU/EEA and the WHO European Region, reported treatment success rates across all cohorts remain well below the targets. Successful treatment outcomes for new and relapsed TB and RR/MDR-TB cohorts were 73.4% and 57.2%, respectively.
In total, 71.7% of the new and relapsed cases reported in the EU/EEA in 2020 had a successful treatment outcome at 12 months in 2021. Treatment success at 24 months for RR/MDR-TB was 51.7%; for pre-extensively drug-resistant (XDR) TB it was 17.0%. Treatment success at 36 months for XDR-TB was 66.7%.
HIV prevalence in TB cases
In 2021, HIV prevalence in incident TB cases was estimated to be 13% – another year with no change after an unprecedented rise from 4% to 12% during the period 2007–2016. There were an estimated 29 000 HIV-positive TB cases in the Region. In the EU/EEA, there were 12 277 cases with known HIV status, 3.8% of which were reported as HIV-positive.
Further efforts are needed to improve the reporting of HIV coinfection, TB in prisons, and treatment outcomes.
Efforts and resources for the future
In the fight against TB, urgent investment in resources, support and care is vital, particularly in the context of the COVID-19 pandemic, which has jeopardized progress towards milestones in WHO’s End TB Strategy.
World Tuberculosis Day is observed on 24 March each year around the world. Its overall goal is to raise awareness about the burden of TB worldwide and the status of TB prevention and control efforts. TB elimination is defined as less than one case of TB disease per 1 million population per year.
Links
Editorial in Eurosurveillance by Andrea Ammon and Hans Kluge: Ending tuberculosis in Europe – resetting the course in the post-COVID-19 era
Tuberculosis surveillance and monitoring in Europe 2023 –2021 data
Political declaration of the UN General Assembly High-Level Meeting on the Fight Against Tuberculosis
ECDC resources
Podcast ECDC: on Air – Episode 34 – Senia Rosales-Klintz – Let’s End TB
Rapid communication: Monitoring the progress achieved towards ending tuberculosis in the EU/EEA
World Tuberculosis Day 2023
Facts about tuberculosis
Online resources on TB
WHO resources
World Tuberculosis Day 2023, campaign materials
Tuberculosis Action Plan for the WHO European Region 2023–2030
WHO Regional Office for Europe – online resources on TB
WHO Regional Office for Europe – publications on TB



