PROVIDENCE, R.I. [Brown University] — To find treatments for connective tissue disorders like fibrosis, scientists need models that can replicate the structure and function of human tissue when it’s healthy as well as when it isn’t, and react to drugs just like diseased human tissue would. But most models are based on animals and present significant limitations.
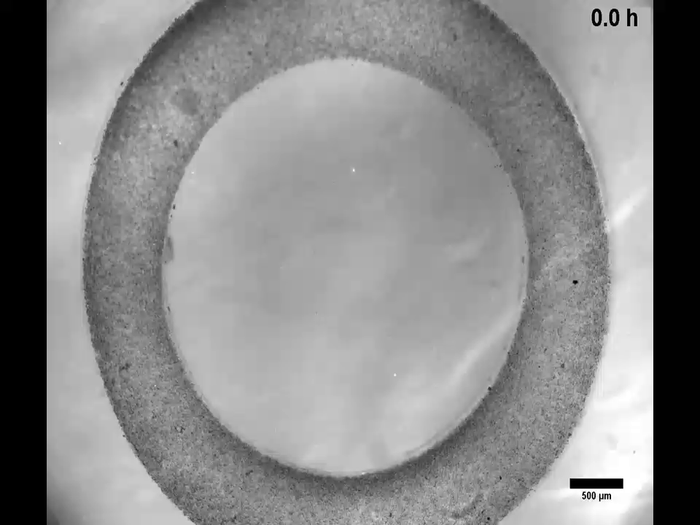
Credit: Courtesy of the Morgan lab at Brown University
PROVIDENCE, R.I. [Brown University] — To find treatments for connective tissue disorders like fibrosis, scientists need models that can replicate the structure and function of human tissue when it’s healthy as well as when it isn’t, and react to drugs just like diseased human tissue would. But most models are based on animals and present significant limitations.
A new laboratory test model developed by Brown University researchers uses human cells and replicates not only the structure of human tissue, but also its mechanics.
The researchers describe the model in an Advanced Science study published on Tuesday, Feb. 1.
“This model gives researchers a new tool to not only explore the underlying mechanisms of fibrosis and inherited diseases of the extracellular matrix but to also test potential treatments for them,” said senior author Jeff Morgan, a Brown University professor of pathology and laboratory medicine, and of engineering.
That development is crucial, Morgan added, because there are no cures for fibrosis, and disorders of the extracellular matrix like Ehlers-Danlos syndrome and Marfan syndrome are in need of new treatments.
Framing the issue
Key to the functionality of the new model is that it does not include an external artificial “scaffold” for the cells; it uses a novel approach in which cells are harnessed to make their own natural extracellular matrix.
Most tissue engineering approaches rely on the use of protein or polymer scaffolds, explained study coauthor Ben Wilks, who earned a Ph.D. in biomedical engineering at Brown and is now a research fellow at Harvard Medical School and Massachusetts General Hospital. Conventional methods involve growing cells on plastic, while newer approaches embed cells in a collagen hydrogel to mimic the extracellular matrix. This new approach goes much further — it allows cells to synthesize and assemble their own human extracellular matrix.
Over the past few decades, there’s been a shift in scientific understanding of the extracellular matrix of tissues. Not only does the matrix provide structural support, but it also communicates with the cells through the transmission of mechanical and biochemical signals. This dynamic, bidirectional communication between matrix and cells plays a crucial role in maintaining cellular homeostasis and tissue function, Wilks said.
“We are interested in how changes in nutrients, growth factors or drug treatments affect cellular synthesis and remodeling of the extracellular matrix and the resulting mechanical properties of the tissue constructs,” Wilks said. “Therefore, a scaffold-free approach is much better suited to study the questions we are asking.”
Researchers in Morgan’s lab at Brown have been investigating scaffold-free tissue engineering for over 15 years. The lab’s focus is on developing tools that allow scientists to build upon the intrinsic properties of cells to assemble 3D tissues and synthesize their own extracellular matrix, Morgan explained. The lab has developed technology that enables researchers to control the 3D shape of the engineered tissue constructs, forming spheres, rings or more complex geometries, by harnessing a phenomenon they call cellular self-assembly.
However, cellular self-assembly seemed to work differently with fibroblasts, a highly contractile cell found throughout the body that plays important roles in wound healing, the synthesis and degradation of extracellular matrix, and tissue homeostasis.
The tissue stiffness that is characteristic of progressive fibrosis, for example, is due to the abnormal behavior of fibroblasts that accumulate and modify the extracellular matrix in a way that ultimately results in a loss of organ function.
When the researchers applied the lab’s technology to fibroblasts, the tissue constructs would spontaneously break.
As a Ph.D. student in Morgan’s lab, Wilks discovered that altering the composition of the nutrients in which the cells were grown would help stabilize the formation of the tissue constructs for days to weeks or even months.
Further, Wilks recognized that by adjusting additional parameters like the mold geometry and number of cells, he could form stable 3D ring-shaped tissue constructs, or models, that facilitated the tension that caused the fibroblasts to self-orient and synthesize their own extracellular matrix.
“That was really when I started to get excited: When I saw how the fibroblasts were aligning and synthesizing this beautiful 3D collagen-rich extracellular matrix in a periodic wave pattern that resembles what you see in native connective tissues like ligaments and tendons,” Wilks said. “I had never seen that before in an engineered tissue construct.”
A test of strength
Wilks wondered if it was possible to quantify the stiffness and strength of the tissue constructs to allow researchers to replicate normal tissue as well as tissue affected by disease.
Using a tensile testing machine called an Instron, the team measured how much force it took to stretch the tissue until it broke. This type of data can be used to assess mechanical properties like the strength and stiffness of the tissues, which can then be related to tissues in the human body. It can also be used to measure how the addition of a drug would alter tissue strength and stiffness.
For example, said Wilks, the data can be used to test whether an anti-fibrotic drug candidate stops the tissue stiffening that is characteristic of fibrotic diseases.
“In this paper, we develop a 3D connective tissue model that enables us to directly quantify how exposing cells in a 3D environment to different nutrients, growth factors or drug treatments results in changes in extracellular matrix synthesis and tissues mechanics, which is an important functional metric of tissues and used clinically to monitor disease progression,” Wilks said. “While there is still a lot of ongoing work, we think this model shows promise for screening potential anti-fibrotic drugs. This would address a major unmet need since there are currently no treatments available that can completely halt or reverse fibrosis.”
The new model is one of the most advanced constructs to represent the 3D architecture, composition and mechanics of native connective tissues like ligaments and tendons, the researchers said. Animal models are expensive, ethically contentious and not always predictive of human pathophysiology, said Morgan, who directs the Brown University Center for Alternatives to Animals in Testing.
He added that this type of research is a valuable stepping stone to creating sophisticated models that can replace and surpass the use of animals.
Journal
Advanced Science
DOI
10.1002/advs.202103939
Method of Research
Computational simulation/modeling
Subject of Research
Cells
Article Title
Quantifying Cell-Derived Changes in Collagen Synthesis, Alignment, and Mechanics in a 3D Connective Tissue Model
Article Publication Date
1-Feb-2022
COI Statement
J.R.M. has an equity interest in Microtissues, Inc. This relationship has been reviewed and is managed by Brown University in accordance with its conflict of interest policies.




