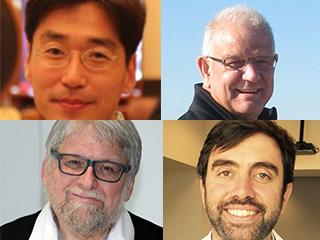
Credit: Baylor College of Medicine
An international team of scientists has discovered that the gene, OGDHL, a key protein required for normal function of the mitochondria — the energy-producing factory of the cell — and its chaperone, nardilysin (NRD1) are linked to progressive loss of neurological function in humans. Working with the fruit fly, an experimental animal model in the lab, the scientists found a mechanism by which misregulation of mitochondrial function leads to neurodegeneration. The results appear in Neuron.
"In our research we look for genes whose loss of function results in deterioration of neurological functions in the fruit fly Drosophila melanogaster," said first author Dr. Wan Hee Yoon, postdoctoral fellow in the laboratory of Dr. Hugo Bellen, professor at Baylor College of Medicine, investigator at the Howard Hughes Medical Institute, and senior author of the paper. "In the fly we found that loss of function of nardilysinled to a slow, progressive neurodegeneration."
Yoon and colleagues discovered that nardilysin helps the folding of an important protein, an enzyme called OGDH, present in mitochondria. Loss of nardilysin function results in loss of OGDH and a build-up of a compound called a-ketoglutarate (a-KG). High levels of a-KG increase a cellular response mechanism called mTOR that normally provides clearance of cellular components such as proteins and organelles. Yoon observed that mutation of nardilysin leads to abnormal build-up of a-KG followed by mTOR activation and eventually to slow accumulation of cellular trash. Importantly, a drug named rapamycin suppresses the neurodegenerative conditions caused by this accumulation of cellular garbage.
In 2009, a group led by Dr. Eiichiro Nishi in Japan genetically engineered a mouse to lack nardilysin.The mice developed neurological problems with motor coordination, balance and memory issues, findings which at the time were not known to be linked to the mechanism described above in the fruit fly. The team led by Bellen realized that the results in fruit flies and in mice might suggest a role for nardilysin and its target protein OGDH in neurological problems in humans.
Searching for disease variants of nardilysin, OGDHL
At the same time that Yoon was investigating nardilysinand its target protein OGDH, across the street co-author Dr. Ender Karaca, a postdoctoral fellow in the laboratory of Dr. James R. Lupski's group at Baylor, was working to solve a rare disease by sequencing the patient's genome through the Baylor-Hopkins Center for Mendelian Genomics (BHCMG). Karaca had discovered a 16-year-old patient with a rare variant in OGDHL who was unable to walk, was bound to a wheelchair and whose head had not grown normally. Yoon and Karaca connected and realized that the mechanism in flies that Yoon was working on might explain the undiagnosed patient of Karaca. "We realized that Ender had identified OGDHL as the top candidate gene for his patient at the same time that we were identifying OGDHL as a target of nardilysin," said Yoon. "After we saw a patient with a severe disorder and variants in OGDHL, we wondered about nardilysin," said Bellen. The researchers then widened their search for similar patients by posting the information of the disease-causing variants of nardilysinin GeneMatcher, a web tool for rare disease researchers developed by the BHCMG team at Johns Hopkins University. Researchers looking for patients carrying rare disease genes post the gene in GeneMatcher. If another researcher around the world has a patient with a matching gene, the teams can contact each other to share the information and collaborate. By posting nardilysinin GeneMatcher, Yoon and colleagues identified a patient whose DNA had been sequenced at the University of California in Los Angeles Clinical Genomics Center. The patient is a 15-year-old boy who presents with symptoms that are remarkably similar to those present in the patient identified by Karaca. "We knew then that these two patients had a very similar disorder, but we had to prove that the genetic variants were causing their conditions," said Yoon and Bellen.
Using flies to study how human disease genes work
The data from the two patients were strong evidence that the variants in nardilysin and OGDHL are linked to neurodegenerative disease in humans. However, to establish that the disease variants can cause the condition, the researchers turned back to the flies where they could use genetic technology to test the variants. "We can test a human gene side by side with a copy containing a variant from a patient in flies," said co-author Dr. Michael F. Wangler, assistant professor of molecular and human genetics at Baylor. Using this technology, Yoon showed that mutant flies carrying a normal copy of the human gene show normal development and neuronal function. However, flies carrying genes with deleterious variants found in patients failed to rescue the loss of the genes in flies. This suggests that the mutations found in patients are indeed deleterious.
"These studies show how valuable the fruit fly model is to uncover and test genes linked to human conditions, and to work out how mutations may cause diseases," said Bellen.
###
Other contributors to this work include Hector Sandoval, Sonal Nagarkar-Jaiswal, Manish Jaiswal, Shinya Yamamoto, Nele A. Haelterman, Nagireddy Putluri, Vasanta Putluri, Arun Sreekumar, Tulay Tos, Ayse Aksoy, Taraka Donti, Brett H. Graham, Mikiko Ohno, Eiichiro Nishi, Jill Hunter, Donna M. Muzny, Jason Carmichael, Joseph Shen, Valerie A. Arboleda, Stanley F. Nelson.
The authors are affiliated with one or more of the following institutions: Baylor College of Medicine, Texas Children's Hospital, Dr. Sami Ulus Research and Training Hospital of Women's and Children's Health and Diseases (Turkey), Kyoto University, Valley Children's Hospital at Madera and the University of California at Los Angeles.
This study was supported by grants from the National Institutes of Health (NIH R01GM067858, NIH T32 NS043124-11) and the Research Education and Career Horizon Institutional Research and Academic Career Development Award Fellowship 5K12GM084897, the Jan and Dan Duncan Neurological Research Institute at Texas Children's Hospital, the CPRIT Metabolomics Core Facility Support Award RP120092, NCI/ 2P30CA125123-09 Shared Resources Metabolomics core, Dan L. Duncan Comprehensive Cancer Center (DLDCC), Alkek Center for Molecular Discovery, Mass Spectrometry COE by Agilent and the NIH R01GM098387. Further support came from research grants 26293068, 26670139 and 26116715 and a research program of the P-Direct from the MEXT of Japan and the NIH K08NS076547 funded by National Institute of Neurological Disorders and Stroke. The authors acknowledge the support of the NIH (1RC4GM096355), the Robert A. and Renee E. Belfer Family Foundation, the Huffington Foundation and Target ALS and the Howard Hughes Medical Institute. This work was also supported in part by a grant from the National institute of Neurological Disease and Stroke (R01NS058529), the Baylor-Hopkins Center for Mendelian Genomics, the US National Human Genome Research Institute, National Heart Lung and Blood Institute grant U54HG006542. J.R.L. has stock ownership in 23andMe and Lasergen, is a paid consultant for Regeneron Pharmaceuticals and is a coinventor on multiple United States and European patents related to molecular diagnostics for inherited neuropathies, eye diseases and bacterial genomic fingerprinting. The Baylor College of Medicine derives revenue from the chromosomal microarray analysis and clinical exome sequencing offered in the Baylor Genetics Laboratory.
Media Contact
Allison Huseman
[email protected]
713-798-4710
@bcmhouston
https://www.bcm.edu/news
############
Story Source: Materials provided by Scienmag





