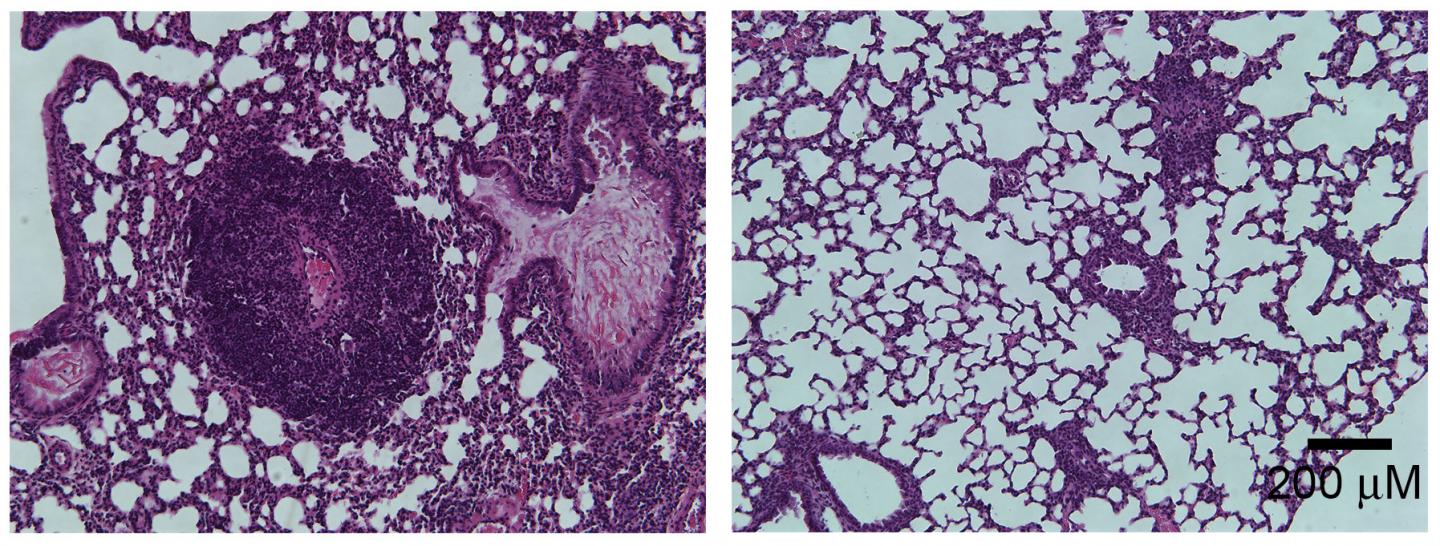
Credit: He et al., 2017
Defects in the body's regulatory T cells (T reg cells) cause inflammation and autoimmune disease by altering the type of bacteria living in the gut, researchers from The University of Texas Health Science Center at Houston have discovered. The study, "Resetting microbiota by Lactobacillus reuteri inhibits T reg deficiency-induced autoimmunity via adenosine A2A receptors," which will be published online December 19 in The Journal of Experimental Medicine, suggests that replacing the missing gut bacteria, or restoring a key metabolite called inosine, could help treat children with a rare and often fatal autoimmune disease called IPEX syndrome.
T reg cells suppress the immune system and prevent it from attacking the body's own tissues by mistake. Defects in T reg cells therefore lead to various types of autoimmune disease. Mutations in the transcription factor Foxp3, for example, disrupt T reg function and cause IPEX syndrome. This inherited autoimmune disorder is characterized by a variety of inflammatory conditions including eczema, type I diabetes, and severe enteropathy. Without a stem cell transplant from a suitable donor, IPEX syndrome patients usually die before the age of two.
Autoimmune diseases can also be caused by changes in the gut microbiome, the population of bacteria that reside within the gastrointestinal tract. In the study, the team led by Yuying Liu and J. Marc Rhoads at The University of Texas Health Science Center at Houston McGovern Medical School find that mice carrying a mutant version of the Foxp3 gene show changes in their gut microbiome at around the same time that they develop autoimmune symptoms. In particular, the mice have lower levels of bacteria from the genus Lactobacillus. The researchers discovered that by feeding the mice with Lactobacillus reuteri, they could "reset" the gut bacterial community and reduce the levels of inflammation, significantly extending the animals' survival.
Bacteria can secrete metabolic molecules that have large effects on their hosts. The levels of a metabolite called inosine were reduced in mice lacking Foxp3 but were restored to normal after resetting the gut microbiome with L. reuteri. The researchers found that, by binding to cell surface proteins called adenosine A2A receptors, inosine inhibits the production of Th1 and Th2 cells. These pro-inflammatory T cell types are elevated in Foxp3-deficient mice, but their numbers are diminished by treatment with either L. reuteri or inosine itself, reducing inflammation and extending the animals' life span.
"Our findings suggest that probiotic L. reuteri, inosine, or other A2A receptor agonists could be used therapeutically to control T cell-mediated autoimmunity," says Yuying Liu.
###
Conflict of interest statement: Some of the authors of this study, including Yuying Liu and J. Marc Rhoads, have a patent application pending on use of inosine and A2A agonists in IPEX syndrome.
He, B., et al. 2017. J. Exp. Med. https://doi.org/10.1084/jem.20160961
About The Journal of Experimental Medicine
The Journal of Experimental Medicine (JEM) features peer-reviewed research on immunology, cancer biology, stem cell biology, microbial pathogenesis, vascular biology, and neurobiology. All editorial decisions are made by research-active scientists in conjunction with in-house scientific editors. JEM provides free online access to many article types from the date of publication and to all archival content. Established in 1896, JEM is published by The Rockefeller University Press. For more information, visit jem.org.
Visit our Newsroom, and sign up for a weekly preview of articles to be published. Embargoed media alerts are for journalists only.
Follow JEM on Twitter at @JExpMed and @RockUPress.
Media Contact
Ben Short
[email protected]
212-327-7053
@RockUPress
http://www.rupress.org/
############
Story Source: Materials provided by Scienmag