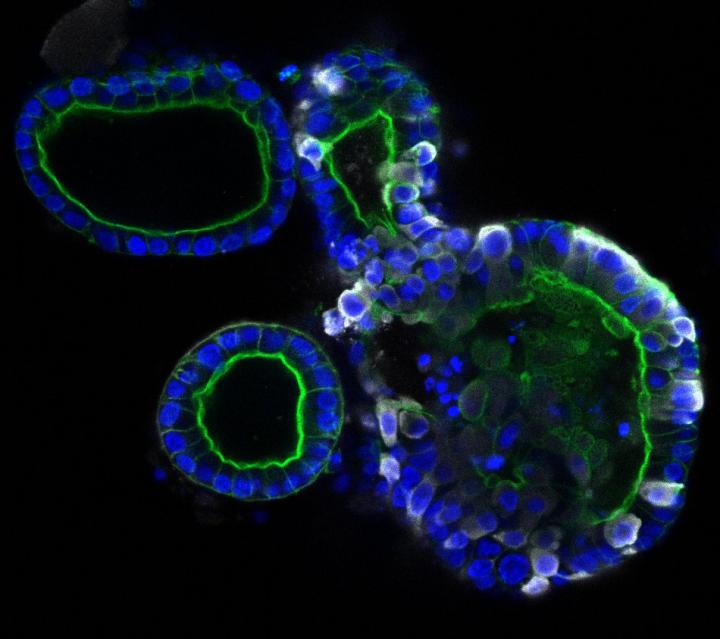
Credit: Joep Beumer, copyright Hubrecht Institue
Researchers from the Hubrecht Institute in Utrecht, Erasmus MC University Medical Center Rotterdam, and Maastricht University in the Netherlands have found that the coronavirus SARS-CoV-2, which causes COVID-19, can infect cells of the intestine and multiply there. Using state-of-the-art cell culture models of the human intestine, the researchers have successfully propagated the virus in vitro, and monitored the response of the cells to the virus, providing a new cell culture model for the study of COVID-19. These findings could explain the observation that approximately one third of COVID-19 patients experience gastrointestinal symptoms such as diarrhea, and the fact that the virus often can be detected in stool samples. The results of this study were published in the scientific journal Science on the 1st of May 2020.
Patients with COVID-19 show a variety of symptoms associated with respiratory organs – such as coughing, sneezing, shortness of breath, and fever – and the disease is transmitted via tiny droplets that are spread mainly through coughing and sneezing. One third of the patients however also have gastrointestinal symptoms, such as nausea and diarrhea. In addition, the virus can be detected in human stool long after the respiratory symptoms have been resolved. This suggests that the virus can also spread via so-called “fecal-oral transmission”.
Though the respiratory and gastrointestinal organs may seem very different, there are some key similarities. A particularly interesting similarity is the presence of the ACE2 receptor, the receptor through which the COVID-19 causing SARS-CoV-2 virus can enter the cells. The inside of the intestine is loaded with ACE2 receptors. However, until now it was unknown whether intestinal cells could actually get infected and produce virus particles.
Intestinal organoids
Researchers from the Hubrecht Institute, Erasmus MC and Maastricht University set out to determine whether the SARS-CoV-2 virus can directly infect the cells of the intestine, and if so, whether it can replicate there as well. They used human intestinal organoids: tiny versions of the human intestine that can be grown in the lab. Hans Clevers (Hubrecht Institute): “These organoids contain the cells of the human intestinal lining, making them a compelling model to investigate infection by SARS-CoV-2.”
Infection of intestinal cells
When the researchers added the virus to the organoids, they were rapidly infected. The virus enters a subset of the cells in the intestinal organoids, and the number of cells that are infected increases over time. Using electron microscopy, an advanced way to visualize different components of the cell in great detail, the researchers found virus particles inside and outside the cells of the organoids. Peter Peters (Maastricht University): “Due to the lockdown, we all studied virtual slides of the infected organoids remotely from home.”
The researchers investigated the response of the intestinal cells to the virus with RNA sequencing, a method to study which genes are active in the cells. This revealed that so-called interferon stimulated genes are activated. These genes are known to combat viral infection. Future work will focus on these genes more carefully, and on how they could be used to develop new treatments.
The researchers also cultured the organoids in different conditions that result in cells with higher and lower levels of the ACE2 receptor, through which SARS-CoV-2 can enter the cells. To their surprise, they found that the virus infected cells with both high and low levels of the ACE2 receptor. Ultimately, these studies may lead to new ways to block the entry of the virus into our cells.
Implications
Bart Haagmans (Erasmus MC): “The observations made in this study provide definite proof that SARS-CoV-2 can multiply in cells of the gastrointestinal tract. However, we don’t yet know whether SARS-CoV-2, present in the intestines of COVID-19 patients, plays a significant role in transmission. Our findings indicate that we should look into this possibility more closely.” The current study is in line with other recent studies that identified gastrointestinal symptoms in a large fraction of COVID-19 patients and virus in the stool of patients free of respiratory symptoms. Special attention may be needed for those patients with gastrointestinal symptoms. More extensive testing using not only nose and throat swabs, but also rectal swabs or stool samples may thus be needed.
In the meantime, the researchers are continuing their collaboration to learn more about COVID-19. They are studying the differences between infections in the lung and the intestine by comparing lung and intestinal organoids infected with SARS-CoV-2.
###
Publication
SARS-CoV-2 productively Infects Human Gut Enterocytes. Mart M. Lamers*, Joep Beumer*, Jelte van der Vaart*, Kèvin Knoops, Jens Puschhof, Tim I. Breugem, Raimond B.G. Ravelli, J. Paul van Schayck, Anna Z. Mykytyn, Hans Q. Duimel, Elly van Donselaar, Samra Riesebosch, Helma J.H. Kuijpers, Debby Schipper, Willine J. van de Wetering, Miranda de Graaf, Marion Koopmans, Edwin Cuppen, Peter J. Peters, Bart L. Haagmans† and Hans Clevers†. Science 2020. DOI
* Equal contribution, † equal contribution.
This study was a collaboration between the Hubrecht Institute in Utrecht, the Erasmus MC University Medical Center Rotterdam, Maastricht University, the UMC Utrecht and Single Cell Discoveries in the Netherlands. The microscopy data are publicly available via the Image Data Resource (idr0083, https:/
Hans Clevers is principal investigator at the Hubrecht Institute and the Princess Máxima Center for Pediatric Oncology, professor of Molecular Genetics at the UMC Utrecht and Utrecht University, and Oncode Investigator.
Bart Haagmans is a principal investigator at the Viroscience department at the Erasmus MC University Medical Center Rotterdam.
Peter Peters is director and principal investigator at the Maastricht Multimodal Molecular Imaging Institute (M4i) and professor of Nano Biology at the Maastricht University and Maastricht University Medical Center.
About the Hubrecht Institute
The Hubrecht Institute is a research institute focused on developmental and stem cell biology. It encompasses 23 research groups that perform fundamental and multidisciplinary research, both in healthy systems and disease models. The Hubrecht Institute is a research institute of the Royal Netherlands Academy of Arts and Sciences (KNAW), situated on Utrecht Science Park. Since 2008, the institute is affiliated with the UMC Utrecht, advancing the translation of research to the clinic. The Hubrecht Institute has a partnership with the European Molecular Biology Laboratory (EMBL). For more information, visit http://www.
About Maastricht University
Maastricht University (UM) is the most international university in the Netherlands and, with 18,000 students and 4,400 employees, is still growing. The university stands out for its innovative education model, international character and multidisciplinary approach to research and education. Thanks to its high-quality research and study programmes as well as a strong focus on social engagement, UM has quickly built up a solid reputation. Today it is considered one of the best young universities in the world.
About Erasmus MC
Erasmus MC is the largest University Medical Center in the Netherlands. Our primary goal is a healthy population. Nearly 14,000 employees devote themselves every day to providing outstanding care, facilitating world-class education and conducting pioneering research. These professionals are instrumental in developing expertise on health and illness. They link the latest scientific insights to practical treatments and prevention measures to provide maximum benefit to patients and to enable healthy people to stay healthy longer. Being visibly better and leading the way in the areas of complex, innovative and acute care by collaborating with others: these are key ambitions at Erasmus MC.
Media Contact
Melanie Fremery
[email protected]
Original Source
https:/
Related Journal Article
http://dx.




