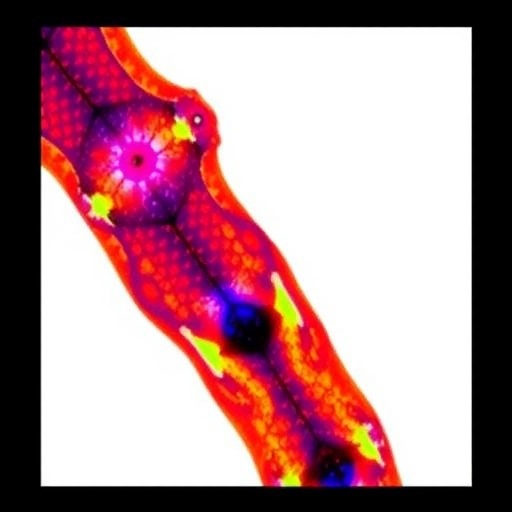
In an innovative leap forward for the field of medical imaging, a recent study published in the Annals of Biomedical Engineering has shed light on the intricate relationships between diabetes mellitus and the condition of cartilage and menisci within the human knee joint. With a focus on advanced imaging techniques, this research reveals critical insights that could transform how clinicians diagnose and manage joint conditions in diabetic patients. T2 mapping, a novel magnetic resonance imaging (MRI) technique, has emerged as a pivotal tool in this endeavor, unveiling detailed information about tissue composition and health.
At its core, this research investigates the potential impact of diabetes on knee cartilage and meniscal structures, both of which play essential roles in maintaining joint stability and function. Diabetes mellitus has long been associated with various musculoskeletal complications, and this study underscores the urgency of understanding how this prevalent metabolic disorder affects joint health. The advent of T2 mapping at a magnetic field strength of 3 Tesla (3T) enables researchers to explore the biochemical milieu of cartilage tissues, providing real-time insights that were previously inaccessible.
T2 mapping, a technique that measures T2 relaxation times within tissues, serves as a powerful non-invasive method to assess cartilage quality. Traditional imaging modalities often fall short in identifying early degenerative changes. This study demonstrates that T2 mapping can detect subtler alterations in cartilage structure and composition, thus allowing for earlier intervention and management of potential joint issues. By focusing specifically on diabetic patients, the researchers aim to fill a vital knowledge gap that has persisted in both clinical and research arenas.
Examining a cohort of diabetic patients, the study presents compelling evidence of altered T2 relaxation times in knee cartilage compared to non-diabetic individuals. The findings suggest that the physiological landscape of cartilage is profoundly affected by diabetes, likely due to metabolic derangements that impact collagen structure and water content within the tissue. These insights not only enhance the understanding of diabetes-related joint changes but also pave the way for tailored therapeutic approaches that could mitigate these effects.
The implications of this research extend beyond academia; they resonate within clinical settings where rheumatologists and orthopedic specialists grapple with the growing prevalence of diabetes among patients presenting with joint pain. The ability to pinpoint cartilage degradation in its nascent stages could revolutionize treatment paradigms. Rather than relying solely on symptomatology, clinicians may soon harness T2 mapping data to inform decision-making, crafting personalized management strategies that focus on preserving joint function and enhancing quality of life.
Moreover, the necessity for regular monitoring of joint health in diabetic patients cannot be overstated. As the incidence of diabetes continues to rise globally, the healthcare system faces an escalating burden of diabetes-related complications, including osteoarthritis and other joint disorders. This study highlights the essential role that state-of-the-art imaging technologies, like T2 mapping, will play in future preventive healthcare initiatives aimed at mitigating these escalating risks.
Throughout the research, rigorous methodological standards ensured the reliability and validity of the findings. A well-defined study cohort, meticulous data collection, and detailed statistical analyses fortified the conclusions drawn. These factors, combined with the advanced imaging capabilities offered by 3T MRI, lend credibility to the assertion that T2 mapping can serve as a benchmark for evaluating joint health in diabetic individuals.
As the medical community continues to embrace technological advancements, the synergy between radiology and endocrinology becomes increasingly evident. This study exemplifies how interdisciplinary collaboration can yield profound benefits for patient care. Radiologists equipped with sophisticated imaging techniques can work alongside endocrinologists and primary care physicians to monitor and address the musculoskeletal complications of diabetes, creating a holistic approach to patient wellness.
In the pursuit of further understanding the complexities of joint health in diabetes, ongoing research will undoubtedly be essential. The promising results of this study serve as a clarion call for continued exploration into the mechanisms underlying cartilage degeneration and the development of effective intervention strategies. Future studies could expand the scope of T2 mapping applications, exploring its utility not only in diabetes but also in other metabolic disorders and conditions affecting cartilage integrity.
Ultimately, the relationship between diabetes and joint health remains a multifaceted challenge that demands attention from researchers, clinicians, and public health officials alike. By leveraging advanced imaging techniques like T2 mapping, the medical community takes a crucial step toward addressing the needs of diabetic patients and altering the trajectory of their long-term joint health outcomes. This cutting-edge research encapsulates the spirit of innovation necessary to confront the growing challenges posed by diabetes, invigorating hope for enhanced patient care.
As the healthcare landscape evolves, tools like T2 mapping pave the way for more precise diagnostics and personalized medicine. The findings presented by Hu et al. not only contribute to the existing body of literature but also ignite conversations around the need for a multidisciplinary approach to managing diabetes-related complications. This emerging field of study holds the potential to transform clinical practices and ultimately improve life quality for millions of individuals living with diabetes.
In conclusion, as we look to the future of diabetes research and treatment, the integration of sophisticated imaging methodologies with clinical practice will be vital. The insights gleaned from T2 mapping may serve as a foundation upon which a new paradigm of diabetes care is built—one that prioritizes early detection, personalized interventions, and holistic patient management strategies, ensuring that diabetes does not dictate the overall health of individuals but rather serves as one of many aspects of a comprehensive health narrative.
Subject of Research: Impact of diabetes mellitus on knee cartilage and menisci assessed through T2 mapping.
Article Title: T2 Mapping at 3 T of Cartilage and Menisci in Patients with Diabetes Mellitus.
Article References:
Hu, N., Liang, X., Zhu, J. et al. T2 Mapping at 3 T of Cartilage and Menisci in Patients with Diabetes Mellitus.
Ann Biomed Eng (2026). https://doi.org/10.1007/s10439-026-03990-5
Image Credits: AI Generated
DOI: https://doi.org/10.1007/s10439-026-03990-5
Keywords: T2 mapping, diabetes mellitus, cartilage health, knee joint, MRI technology, metabolic disorders, personalized medicine, musculoskeletal complications.
Tags: 3T T2 mapping in diabetesadvanced medical imaging in diabetesbiochemical analysis of cartilagecartilage health in diabetic patientsdiabetes impact on joint healthinnovative imaging techniques for cliniciansknee joint stability and functionmenisci imaging techniquesMRI for joint conditionsmusculoskeletal complications of diabetesnon-invasive cartilage assessmentT2 relaxation times in tissues