In a groundbreaking study published in the Journal of General Internal Medicine, researchers led by Hynes et al. investigated the impinging factors surrounding 30-day mortality rates following diagnostic coronary angiography, a critical procedure used extensively to diagnose coronary artery disease. This comparative analysis focused on two contrasting healthcare environments: the Veterans Affairs (VA) hospitals and community hospitals. The implications of the findings could herald significant changes in clinical practice and healthcare policy, particularly in terms of resource allocation and patient care protocols.
Coronary angiography, a procedure that employs X-ray technology to visualize the blood vessels of the heart, has long been a cornerstone in the diagnostic arsenal for cardiovascular diseases. However, understanding the mortality outcomes associated with this procedure in different hospital settings provides keen insights into the quality of care and patient outcomes. The notion that healthcare delivery varies considerably between different institutions is well-established, but this study aims to quantify those differences concerning mortality rates.
The study encompassed a considerable sample size, drawing from a comprehensive dataset that included both VA and community hospitals. By performing a meticulous analysis, the researchers sought to determine whether patients receiving diagnostic coronary angiography within these varying environments experienced differing rates of mortality within a crucial 30-day window post-procedure. This 30-day frame is often utilized in medical studies as it encapsulates a critical period for patient recovery and subsequent health decline, if any.
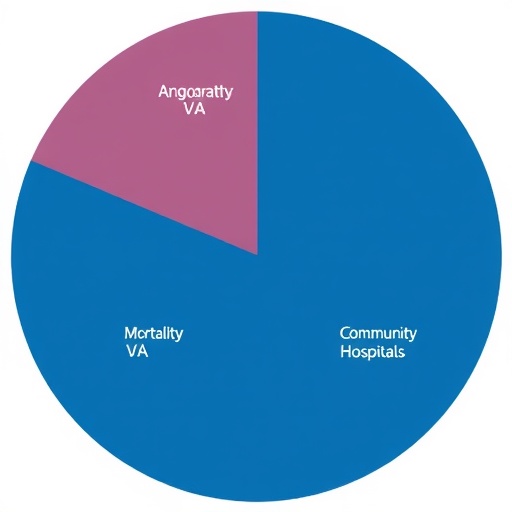
A primary conclusion from the study revealed that patients treated at community hospitals exhibited a noticeably higher 30-day mortality rate compared to those treated at VA hospitals. This finding prompts a broader question about the varying levels of care, follow-up support, and resource availability that might contribute to these disparities. VA hospitals, known for their specialized cardiovascular services and veteran-focused care frameworks, may offer a level of continuous support and follow-up that community hospitals struggle to match.
Further analysis revealed that several variables, including patient demographics, comorbidities, and other health determinants, could significantly influence mortality rates. For instance, patients treated in community hospitals were often older and had a higher prevalence of comorbid conditions that could complicate their post-procedural recovery. Adjusting for these factors, however, did not entirely account for the stark differences observed in mortality rates, thus indicating systemic issues possibly inherent in the healthcare services offered at community hospitals.
Another notable aspect analyzed in the study was the role of healthcare disparities, reflecting upon how socioeconomic factors, access to care, and the quality of healthcare services interact to influence patient outcomes. VA facilities tend to be integrated systems universally serving specific communities, often allowing for a more cohesive approach to patient management, especially concerning chronic conditions prevalent among veterans. This is quite distinct from community hospitals that serve a broader population base with a diverse range of healthcare needs, often lacking the specialized services seen in VA settings.
The study also addressed the clinical significance of comprehensive post-procedural care, emphasizing how patient follow-ups, medication adherence, and lifestyle interventions can critically shape recovery trajectories. It pointedly analyzed the coordination of care in VA hospitals, where follow-up visits and continuous health monitoring are emphasized—a stark contrast to the often fragmented care experienced in community hospitals. Through this lens, it becomes evident that investing in comprehensive care pathways capable of bridging these gaps may influence patient outcomes positively.
Researchers did not shy away from addressing the implications of their findings directly. They posited that there needs to be a concerted effort among healthcare policymakers to enhance quality measures and patient care standards in community hospital settings. These changes could potentially align those standards closer to the ones felt and experienced at VA hospitals. The study advocates for local health systems to engage in quality improvement initiatives that focus on reducing 30-day mortality rates through refined post-discharge care protocols, emphasizing continuity and coordination amongst healthcare providers.
In drawing conclusions, Hynes et al. reinforced the notion that a systematic understanding and response to healthcare inequities can lead to substantial improvements not only in mortality statistics but also in the overall quality of life for patients across various demographics. Their research serves as a crucial touchstone for future studies aimed at unraveling the complex interplay between healthcare accessibility, quality, and outcomes.
As the study continues to make waves within the medical community, it underscores the need for further research to build upon these findings. Future inquiries could expand on various patient groups, exploring intersections with social determinants of health and their implications for elective surgical procedures, diagnostics, and patient management strategies across varying healthcare settings.
In summation, the research by Hynes and colleagues not only sheds light on the troubling disparities between community hospitals and VA facilities regarding 30-day mortality rates after diagnostic coronary angiography but also emphasizes the profound effects that systemic healthcare differences can impose on patient outcomes. As the medical field advances towards a more patient-centered approach, the outcomes of this study may serve as a rallying point for change, potentially sparking a paradigm shift in how healthcare is delivered across the United States.
The advocacy for enhanced quality of care procedures places this research at the forefront of a vital discussion that connects clinical outcomes to healthcare policy. The call for increased investment in community healthcare services could ultimately lead to improvements that bridge the gaps identified, ensuring that all patients, regardless of their healthcare setting, receive equitable and effective care.
Subject of Research: Comparison of 30-Day Mortality After Diagnostic Coronary Angiography at VA and Community Hospitals.
Article Title: Comparison of 30-Day Mortality After Diagnostic Coronary Angiography at VA and Community Hospitals.
Article References: Hynes, D.M., Govier, D.J., Hickok, A. et al. Comparison of 30-Day Mortality After Diagnostic Coronary Angiography at VA and Community Hospitals. J GEN INTERN MED (2026). https://doi.org/10.1007/s11606-025-10110-x
Image Credits: AI Generated
DOI: https://doi.org/10.1007/s11606-025-10110-x
Keywords: Mortality rates, coronary angiography, Veterans Affairs hospitals, community hospitals, healthcare disparities.
Tags: 30-day mortality ratescardiovascular disease diagnosticsclinical practice implicationscommunity hospitals comparisoncoronary angiography outcomesdiagnostic coronary artery diseasehealthcare delivery differenceshealthcare policy changesmortality outcomes in hospitalspatient care protocolsresource allocation in healthcareVeterans Affairs hospitals analysis